- When Life at Memorial Changed
- Clinical Steering Committee Spearheads Memorial's Response
- Critical Care: A Transition to Crisis Management
- Emergency Departments Pivot New Processes for COVID
- Graduate Medical Education Residents Answer the COVID Call
- Nurse Residents Experience Once-In-a-Lifetime Training
- Memorial Meets CB Smith Testing Site Challenges
- The Move to Telehealth
- iPads for Patients, Triage in Tents
- CB Smith Park: The Clinician Experience
- Protecting Vulnerable Nursing Home Residents
- When COVID‑19 Arrived, Donors Stepped Up
- A Quick Pivot to Reach the Community
- Community Services Responds to COVID‑19
- Office of Human Research Takes Action on COVID
- Financial Report: The Effects of the Coronavirus Pandemic
- Life After COVID: Memorial Rehabilitation Institute Leads the Way

LEADING THROUGH

When Life at Memorial Changed
At Memorial Healthcare System, the impact of the COVID‑19 pandemic struck different people at different times.
Memorial Cancer Institute Medical Director Brian Hunis, MD, and Vice President Vedner Guerrier saw reports from China and Italy early on. “We decided: This is happening. We need to get on it,” Mr. Guerrier said.
In March, Khaulah Brice, Director of Emergency Services at Memorial Regional Hospital South, noticed the coronavirus dominating the news. She worried about her 20-year-old son, who played professional soccer in Europe. Would he be at risk for it over there?
For Dawn Broksch, Administrative Director at Memorial Rehabilitation Institute, it suddenly hit home “when we realized we had to stop letting our patients have visitors.”
At Memorial Hospital West, Family Birthplace Director Mary Roberts will always remember St. Patrick’s Day, when she went to help out in the hospital’s Emergency Department. “We were so busy,” she said. “That’s when I knew it was really blowing up.”
The opposite was happening at Memorial Neuroscience Institute. NeuroInterventional Surgeon Brijesh P Mehta, MD, and his team noticed a decrease in patients seeking medical care for strokes. “They were nervous about the virus and waiting too long to come to the hospital,” Dr. Mehta said. “By the time they arrived, they were outside the treatment window.”
For Home Health Administrator Meryl Comiter, COVID became real when patients started saying they were reluctant to have anyone visit them, even trusted home health aides.
Reality shifted at Memorial’s Office of Human Research, too. The team knew they needed to get on the Expanded Access Protocol for the antiviral drug Remdesivir as soon as possible, and Memorial became the first site in South Florida to offer patients the drug as part of a research study.
And for numerous caregivers across the system, outpatient operations shut down and ER visits dropped.
The fourth quarter of fiscal year 2020 at Memorial was dominated by the once-in-a-century experience known as COVID‑19. During those months, it became clear how – and how well – Memorial would deal with the challenge. The system had already stockpiled PPE to respond to emergencies like hurricanes, terror attacks, and yes, pandemics. Now, Memorial’s longtime leadership in the areas of safety, quality and service would provide it with opportunities to rise to the occasion on every level. And Memorial did.
Telehealth expanded: Memorial Cancer Institute and Memorial Physician Group quickly transitioned to nearly all-virtual consultations. Outpatient Services held 3,000 online patient visits in April alone. Home Health revamped its staff schedule to prioritize certain visits. The FDA approved Remdesivir for emergency use, and Memorial received an early large supply thanks to Memorial’s research trial participation. Dr. Mehta made a video PSA, encouraging the community to visit Memorial ERs in the event of stroke. Memorial Rehabilitation Institute took its first steps to becoming the rehab provider of choice for COVID‑19 survivors. And Khaulah Brice’s son not only came back safely to the US, he returned again to Europe – missing international travel bans both times.
Those are just a few stories of how Memorial’s Healthcare Heroes experienced the first days of COVID‑19. Here, in this special section, are more.
Caregivers Take a Moment to Breathe
As the COVID pandemic progressed, prayer groups allowed frontline staff and other members of the Memorial family to take much-needed breaks for their mental and spiritual health. The prayer groups, which began in April at Memorial Hospital West and also were held at Memorial Hospital Miramar, continue to offer welcome moments of calm and support.

Clinical Steering Committee Spearheads Memorial’s Response

The main requirement for a successful pandemic response? A clear clinical and executive command structure to lead it. By early March, Memorial’s newly established Clinical Steering Committee – led by Stanley Marks, MD, FACS, Senior Vice President and Chief Medical Officer – began laying the groundwork to plan and manage all clinical aspects of Memorial’s handling of COVID.
“We were looking at what they were going through in New York and thinking, wow, this is pretty steep,” Dr. Marks said. “We knew we needed to have enough equipment to keep our people safe. So we just full-bore conserved all our PPE, and developed our strategies and policies so that when the spike hit in April, we were ready.”
In addition to Dr. Marks, members of the committee included Paula Eckardt, MD, Chief, Division of Infectious Disease; Rachel Guran, Director, Epidemiology and Infection Control; Maggie Hansen, Senior Vice President and Chief Nurse Executive; Frederick Keroff, MD, Medical Director, Emergency Services; Tom Macaluso, MD, Vice President and Chief Quality and Patient Safety Officer; Aharon Sareli, MD, Chief, Adult Critical Care Services; and Natasha Strokin, Director, Emergency Preparedness.
This “COVID‑19 Command Center Team” met virtually at least once a day for weeks – which later turned into months – to deliberate, establish priorities, and develop guidelines and protocols for the entire healthcare system. The committee regularly communicated their established recommendations to Memorial leadership for implementation at all facilities.
“Basically, the COVID pandemic was like the Olympics for infectious disease,” said Dr. Eckardt. “Even though we knew a pandemic would happen at some point, the coronavirus was completely different in the way it spread worldwide. We had to be on our toes regarding the recommendations we made because we were learning about the disease on the go.”
Committee members worked constantly, reviewing data, speaking with other providers, and continually making and revising decisions. Many times, this work involved reading and analyzing different strategies from all over the world, which were becoming available at a rapid pace.
“We’re not used to following any data that is not peer-reviewed, and a lot of the publications were fast-tracked,” Dr. Eckardt said. “We were very careful in determining what recommendations we were going to follow. Anything that was evidence-based was what we were going to do.”
Physicians on the COVID‑19 Command Center Team performed all of their duties on top of their regular responsibilities, such as seeing patients and being on call. But working closely as a committee was key to Memorial’s overall COVID response.
“I think Memorial has been a leader in how to manage a hospital system in a pandemic,” Dr. Eckardt said.
“Memorial has been a leader in how to manage a hospital system in a pandemic. Other systems look to what we’re doing, because we make decisions very carefully and in a very organized way.”Paula Eckardt, MD
Chief, Division of Infectious Disease

Critical Care: A Transition to Crisis Management

Understanding the sheer scale of the COVID‑19 threat, Memorial’s Critical Care team mobilized to create new workflows, clinical care pathways and safety protocols. The leaders had to prepare to tackle never-before-seen challenges.
“For the first time in history, we needed to ready our system for a true public health crisis with very little data about the disease we were facing,” said Aharon Sareli, MD, Chief, Adult Critical Care Services and Chief Physician Executive, Memorial Physician Group. “As new data continued to emerge, flexibility was of the utmost importance. We had to maintain the ability to make rapid changes in protocols, procedures and treatment pathways.”
Memorial could respond quickly because of its strong critical care team and its experience in seamless transition to “crisis mode,” Dr. Sareli believes. “Dealing with recurring natural catastrophes like hurricanes meant that we had the kind of framework that’s pivotal to crisis management,” he said. “Furthermore, having a core group of dedicated critical care specialists has proved invaluable.”
That critical care team is part of Memorial Physician Group (MPG), Memorial’s network of 305 multispecialty, system-employed physicians. At the onset of the pandemic, they worked around the clock to develop safety guidelines for interacting with COVID patients and to implement new COVID treatment protocols. In collaboration with Memorial’s Office of Human Research, key clinical trials – involving treatments such as Remdesivir and convalescent plasma – were included in ICU care pathways.
Importantly, the ICU team developed new staffing models that allowed ICU specialists (intensivists) to lead other providers and enable them to participate in ICU patient care. Advanced-practice providers from MPG divisions of cardiology, general surgery, trauma and neurosurgery, plus senior internal-medicine residents, were deployed to Memorial’s ICUs. These healthcare providers worked under the supervision of intensivists and greatly assisted in surges of critically ill COVID‑19 patients. Memorial anesthesiologists and nurse anesthetists contributed to COVID‑19 care by forming “line and intubation teams,” helping to place COVID‑19 patients on mechanical ventilation (when needed) and facilitating venous and arterial lines – thereby freeing up the intensivists to focus on providing clinical ICU management.

As Memorial’s ICU areas began to exceed their original bed capacity, the need arose to convert non-ICU areas to provide additional space for critically ill patients. “This only happened with razor-sharp coordination among physicians, nurses, pharmacists, respiratory therapists and administrators,” Dr. Sareli said.
The pandemic has taken a toll on ICU caregivers – particularly as Memorial tightened its visitor restrictions.
“We were already dealing with massive ICU patient volumes, burdens of PPE, unfamiliar geography of the new areas and extremely unstable patients,” Dr. Sareli said. “Then our staff had to face the additional emotional burden of supporting patients and families who had to remain apart.”
Although the pandemic continues, Critical Care continues to step up, Dr. Sareli asserts.
“Our response has exemplified maximum effort and ongoing total commitment,” he said. “I couldn’t be more proud of the team, all of whom have operated under extreme physical and emotional pressure.”
“Our response has exemplified maximum effort and ongoing total commitment. I couldn’t be more proud of the team, all of whom have operated under extreme physical and emotional pressure.”Aharon Sareli, MD
Chief, Adult Critical Care Services and Chief Physician Executive, Memorial Physician Group

Emergency Departments Pivot to New Processes for COVID

As the realities of the coronavirus pandemic became apparent, Memorial made quick changes to patient flow processes in ERs across the healthcare system.
“It was clear COVID wasn’t going to be merely like a bad flu season,” said emergency medicine physician Adam Rubin, MD, “so we knew we had to take our Emergency Department operations to a different level.”
The most immediate task was to isolate COVID from non-COVID patient populations. That meant pitching outdoor, temperature-controlled tents with triage personnel and medical equipment to serve as extensions of Memorial ERs. Via the tent setups, Memorial was able to transfer COVID-positive patients to areas of the hospitals reserved exclusively for them, while ensuring that non-COVID patients could still get the emergency care they required. ER teams also had to keep all Memorial patients and caregivers safe throughout the process.
Memorial’s executive team and Clinical Steering Committee tapped Khaulah Brice, Director, Emergency Services, Memorial Regional Hospital South, to serve as coordinator for the effort across the hospitals.
“The first thing we did was mobilize our protective gear for our caregivers,” she said. “At the time, there wasn’t a lot known about COVID except that it involved the respiratory system. We just knew that staff had to be protected.”
To standardize ER processes at all hospitals, Emergency Department directors began meeting every day to iron out any procedural differences and compare notes about the coronavirus symptoms they were seeing.
“We changed our processes nearly every day for the first two weeks,” Ms. Brice said. “We were looking for what worked best and protected everybody at the same time. Fortunately, our ER teams have very adaptive personalities, and we built very trusting relationships. We were going to be safe, and we were going to be flexible.”
The keys to managing the tents system successfully: complete transparency with both patients and staff, clarity of communication, and treating COVID as a chance to learn, Ms. Brice said.
“Memorial has very high-performing teams in our ERs, and I wouldn’t change anything about the opportunities we had to grow and be better,” she said. “I don’t think there was a challenge that we didn’t handle and learn from.”
“It was a giant undertaking, one we had to do to keep everyone in our hospitals safe,” Dr. Rubin added. “As a system, Memorial did a really good job of staying ahead of the curve.”

Graduate Medical Education Residents Answer the COVID Call

When the coronavirus pandemic began in South Florida, Memorial had a built-in reserve of physicians ready to help where needed: its classes of residents in Graduate Medical Education. Physicians in training were deployed to areas like ICUs and infectious disease – and, prominently, to the COVID‑19 testing site at CB Smith Park.
Memorial residents helped staff CB Smith seven days a week, working on-site to test patients, and making follow-up calls to those who had tested positive. Residents also conducted numerous telehealth consultations with high-risk and COVID-positive patients who remained at home, to monitor their progress and coordinate their care.
“Our residents received an excellent learning experience because they were able to see how COVID was managed both in the hospitals and at patients’ homes,” said Saima Chaudhry, MD, MSHS, Vice President for Academic Affairs and Chief Academic Officer, Graduate Medical Education. “Telehealth was a major initiative for us, and they did an amazing job.”
COVID‑19 significantly changed the entire residency experience. None of Memorial’s trainees had expected to be spending their residencies dealing firsthand with a historic global pandemic.
“Something like this really makes you think about your professional ethos and your responsibilities,” Dr. Chaudhry said. “This is a situation where you’re dealing with a serious new disease, that required all of us to take a risk we never anticipated.”
To support residents through COVID‑19, the GME program instituted a policy of frequent communication, including regular meetings and updates, instructions on PPE, and training on the unique challenges of telehealth, among other topics. The goals: Keep trainees informed of all aspects of Memorial’s response to the pandemic, help them understand their roles in it, and protect their health and safety at all times.
Residents will feel the impacts of the coronavirus pandemic their entire careers, Dr. Chaudhry believes.
“They’ve had to think deep and hard about what it means to be a doctor, and the sacrifices that are involved,” she said. “Our residents are training at a time when there are no practicing physicians in the US who have gone through a pandemic in training. It’s an honor to be able to do this kind of heroic work – a frightening honor.”
“Our residents received an excellent learning experience because they were able to see how COVID was managed both in the hospitals and at patients’ homes.”Saima Chaudhry, MD, MSHS
Vice President for Academic Affairs and Chief Academic Officer, Graduate Medical Education

Nurse Residents Experience Once-In-a-Lifetime Training

When Memorial concluded its first two Nurse Residency Program cohorts in August 2019, nobody had the word “coronavirus” on their minds. By early 2020, nurse residents at Memorial found themselves training for their careers in the midst of a historic pandemic. It required some fast pivots for a program that was created to fill knowledge gaps as baby boomer nurses retired.
“It’s already crucial to fill those gaps because we’re seeing more and more patients who require high-tech and complex care,” said Maggie Hansen, RN, BSN, MHSc, Senior Vice President and Chief Nursing Executive. “And then COVID‑19 hit, and it just compounded that problem tremendously.”
The challenge: Conduct the usual evidence-based curriculum – designed by Memorial’s residency partner, the Vizient/American Association of Colleges of Nursing (AACN) Program – while at the same time accommodating the overwhelming needs of the pandemic.
“It was ‘all hands on deck’ to get through the crisis,” Ms. Hansen said. “Thankfully, that’s not something nurses are afraid to do.”
Physical distancing and other preventive measures placed a number of restrictions on the residency program’s methodologies. Although the program was developed around a group cohesion model that includes significant classroom learning, the residency leaders quickly shifted the approach to e-learning modules and leveraged technology to facilitate meeting the objectives of the residency curriculum. The new COVID clinical environment was also utilized as a real-life platform for learning about the flexibility often necessary in the unpredictable hospital settings where the novice nurses are launching their careers.
“We needed to develop new methodologies spontaneously and expeditiously,” Ms. Hansen said. “There’s no doubt that we’re writing history with this pandemic.”
Another major concern was the physical, emotional, spiritual and intellectual well-being of all nurses on the front lines of COVID. Memorial immediately moved to provide support, including arranging for housing options, shopping services and day care, organizing prayer services, and dedicating resources for self-care, such as bringing in Memorial’s Integrative Medicine experts to promote mindfulness practices.
The pandemic forced Memorial to delay the arrival of the seventh cohort of nurse residents until fall 2020. Going forward, the program will need to continue to adapt itself to changing circumstances, Ms. Hansen explained.
“It’s clear that the coronavirus will not soon be going away, so we’ll keep on making adjustments to the program to ensure that we can impart the same knowledge to residents that we always would,” she said.
And learning the ropes in a crisis like the magnitude of COVID‑19 might have a silver lining or two, Ms. Hansen added.
“The pandemic requires our wonderful novice nurses to build skills like flexibility and teamwork, and helps them learn how to manage rapid change,” she said. “Their infection-control skills will be far and above what they might have been, which will help protect them in the future. These are important lessons. If we pause and reflect on each of them, the history we’re creating now is one from which the future will benefit.”
“It was ‘all hands on deck’ to get through the crisis. Thankfully, that’s not something nurses are afraid to do.”Maggie Hansen, MHSc, RN, BSN
Senior Vice President and Chief Nurse Executive
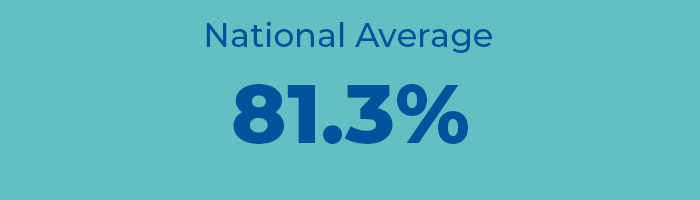
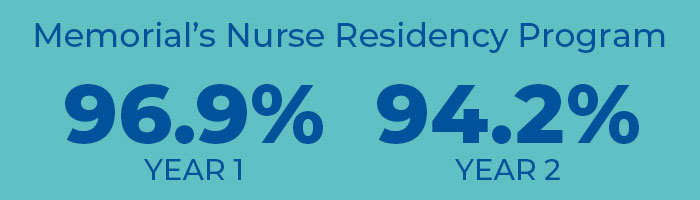
High Retention, High Scores Mark First Years of Residency Program
Just two years in, Memorial’s Nurse Residency Program can boast very high retention rates, pandemic or no pandemic. With the national retention average standing at 81.3 percent, Memorial’s program scored a 96.9 percent rate in its first year and a 94.2 percent rate in its second. In an end-of-program survey of nurse residents in cohorts 1 and 2, respondents consistently rated Memorial above Vizient benchmarks in areas such as ensuring safety, fostering feelings of value and accomplishment, and promoting self-awareness, satisfaction and confidence. Nurse residents also gave glowing ratings to Memorial’s preceptors, scoring them well above Vizient benchmarks in every category.

NURSE RESIDENCY RETENTION RATES

Memorial Meets CB Smith Testing Site Challenges



On most days in CB Smith Park in Pembroke Pines, families would be cycling, jogging, picnicking, playing tennis and shooting hoops. But in March of 2020, the park became a different kind of vital community resource as Gov. Ron DeSantis designated it Florida’s first COVID‑19 drive-through testing site – and asked Memorial Healthcare System to partner with the Florida National Guard, the Broward Sheriff’s Office, Pembroke Pines Police and Quest Diagnostics to make it happen. A truly collaborative effort, the CB Smith operation involved Memorial nurses, clinicians, the system’s supply chain, and especially Memorial’s IT team, which found itself facing a unique challenge to get the test site up and running quickly.
“We approached it in the spirit of: How can we attack this virus from a technology standpoint?” said Jeffrey Sturman, Senior Vice President and Chief Information Officer. “To keep the operation running, we needed to be innovative.”
The site began by providing COVID tests to patients who were symptomatic, and was later expanded to test all South Florida adult residents – regardless of whether they exhibited symptoms – children, and those with previous positive tests who required retesting.
From the start, Memorial’s IT team focused on streamlining the process, so that patients could easily register, get tested, and then hear the results, whether positive or negative, in a reasonable amount of time. In the testing site’s first week, patients’ wait times to book appointments were reduced from hours to less than 30 minutes.

The next challenge was to communicate results. To contact patients who tested negative, the IT team worked with Cisco Systems and CDW Corporation to create an automated calling system. Those with positive results – approximately 16 percent of those tested at the time – received non-automated calls.
Memorial’s IT team ensured connectivity and facilitated all technology setups for the site’s staffing, patient registration and workflow. Throughout the setup process, in addition to the community partners and the National Guard, IT worked closely with Memorial Physician Group and Jennifer Goldman, DO, MBA, Medical Director, Memorial Primary Care, who served as the on-site director of operations.
By April 30 – the end of the fiscal year – the CB Smith team had collected 20,692 COVID tests, 19,375 of which were returned with results. By May, testers at CB Smith Park were testing an average of 800 patients a day, Mr. Sturman said. By September 4, the team had collected more than 109,000 COVID tests at CB Smith Park.
“The silver lining of the COVID pandemic is that when you’re in a state of emergency like that, you’re doing things that typically would take you months of planning. In the world of IT, that means that we can become the benefactors of innovative things that we might not have been doing otherwise.”Jeffrey Sturman
Senior Vice President and Chief Information Officer

The Move to Telehealth

The onset of COVID‑19 presented Memorial with an enormous task: how to move the system en masse from in-person care to virtual platforms. Memorial responded with a massive collaborative effort that involved IT, executives, physician leaders, vendors, and more.
“It definitely took a village to move this forward,” said Bill Manzie, Administrative Director of Telehealth.
As COVID was rapidly advancing, time was short. Within the span of two to three weeks, Memorial provided 358 healthcare providers and their staffs with telehealth training, and additionally trained more than 100 employed physicians on MemorialDOCNow to help reduce wait times.
Memorial also provided patients with crucial education – what telehealth was, and how they could access it on a variety of devices. Some also needed help setting up Memorial MyChart accounts for the first time.
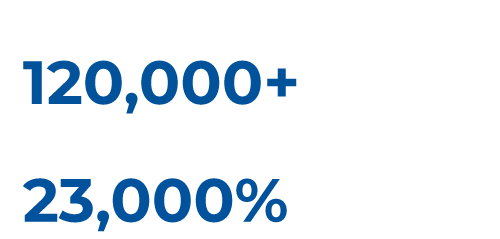
The unprecedented effort showed immediate dividends, and has continued to do so. In the first months of the pandemic alone, Memorial conducted 35,000 telehealth visits. And to date, Memorial has conducted more than 120,000 virtual visits in calendar year 2020 – an eye-popping 23,000% increase over all of 2019.
It’s also pointed the way toward the future. While Memorial’s response was initially focused on the pandemic emergency, it was also a logical outgrowth of technological innovations that Memorial had already been exploring. For example, before COVID, Memorial was in talks with the healthcare technology company Talis Clinical for remote monitoring of cardiac patients receiving ECMO (extracorporeal membrane oxygenation). Now, Memorial is continuing with plans to expand Memorial’s remote patient monitoring opportunities – and is investing heavily into telehealth programs that will make care as accessible and frictionless as possible for both patients and providers.
“Although it was the COVID pandemic that jump-started the importance of telehealth for us, we’re now thinking beyond the pandemic to develop additional options with sustainability in mind,” Mr. Manzie said.
“We are continuing to push this forward as another example of ways new technologies can facilitate patient care,” said Jeffrey Sturman, Senior Vice President and Chief Information Officer. “Stay tuned.”
“Our overall goal with telehealth was and is very simple: Provide patients with the same quality of care that they would have received if they were seeing us in person.”Bill Manzie
Administrative Director of Telehealth
Snapshot: One Telehealth Experience
When Memorial shifted from in-person to virtual visits, all care was affected – and different challenges presented themselves in various areas across the organization.
For example, at Memorial Cancer Institute, patients needed to be accommodated at various stages of their treatment – which meant retooling individual schedules and modifying visits to ensure that care continued uninterrupted, even if not in person. And for patients who still had to come in for chemotherapy or radiation, it meant no visitors.
“Limiting visitors was not popular,” said Vedner Guerrier, Vice President, Oncology Services, “but in the end, our patients were thanking us. Cancer doesn’t pause during a pandemic. They knew that when they could, they were still going to see us via telehealth.”

iPads for Patients, Triage in Tents


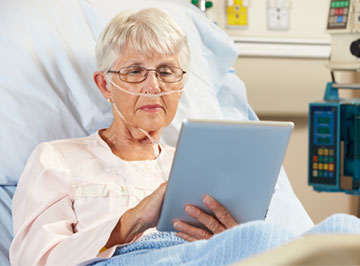
Within Memorial, IT stepped up its technology across the system to connect patients and families with their physicians, caregivers and health facilities in the pandemic.
Fifty iPads were distributed to COVID patients, with dedicated lines that kept them connected to providers even if they felt too unwell to type and swipe. Arming patients with iPads also meant that nurses and other clinicians could communicate with them in non-emergency situations without having to physically enter their rooms – which helped conserve PPE as well.
At Memorial’s other hospitals, more than 250 sharable iPads kept patients in communication with their family members, with hundreds more scheduled for distribution.
When extra space became necessary for triage operations, every Memorial facility responded by setting up air-conditioned tents outside their emergency departments, where they could process and separate COVID and non-COVID patients. At every location, the tents’ construction required technology that seamlessly linked to the hospitals’ existing systems – a logistical challenge that IT helped Memorial meet.
“The Memorial IT project management team and our IT on-site hospital-based teams were heavily involved in setting up the technology that our clinicians needed to process COVID patients efficiently, and to protect other patients in our hospitals at the same time,” said Jeffrey Sturman, Senior Vice President and Chief Information Officer.

CB Smith Park: The Clinician Experience

The COVID‑19 drive-through testing site in CB Smith Park called upon the dedication and expertise of Memorial’s clinicians – a collaborative effort that Jennifer Goldman, DO, MBA, Medical Director, Memorial Primary Care, was asked to spearhead.
“The moment I first showed up on March 19, I realized the magnitude of the testing site and the scope of work that would be required to make it happen,” she said. She proceeded to organize a work group of Memorial Physician Group members, as well as physicians from Memorial Primary Care, oncology and other areas of the organization, to establish and implement testing protocols, quality control, and a positive patient experience.
One of the first challenges was making sure the testing site had enough supplies, which a partnership with Quest Diagnostics resolved by ensuring supplies were delivered directly to CB Smith. Another foe, as the spring weather warmed up, was the heat. Memorial’s CB Smith team set up cooling tents and organized shifts no longer than 90 minutes, so that nurses and others working in layers of PPE had the chance to rest and refresh.
“We created a handbook of protocols for preventing heat stroke and stress at COVID testing sites,” Dr. Goldman said. “Our handbook, which we produced with the Florida Division of Emergency Management, has been given out to test sites all across the country.”
Another key component of the CB Smith effort was following up with positive-testing patients – promptly, efficiently and personally. While patients with negative results were contacted via robocalls, those with positive results received a series of one-on-one follow-up calls from Memorial clinicians. From mid-March to the end of April, the team made 4,007 calls to patients who had tested positive at CB Smith.
“We asked them questions and made sure they knew what to do, like isolate,” Dr. Goldman said. “If they were high-risk – if they had diabetes or another chronic condition – we started them with a free telehealth consultation so we could see what their symptoms were and whether they needed to be linked to a primary care physician. We were able to keep a lot of positive-testing patients from making unnecessary trips to the ER that way.”
Since the testing site opened in March, the Memorial team has held nearly 1,200 telehealth consultations with high-risk patients to date. And the work goes on – but not without rewards for those performing it.
“Clinically, it’s been a great experience, particularly for our residents,” Dr. Goldman said. “From a medical and clinical care standpoint, it’s been eye-opening: To see how ill patients can become from this virus, and how anxiety-provoking it is for people. Our residents have learned firsthand that a comforting, personal phone call from a physician can never be overrated.”
“The moment I first showed up on March 19, I realized the magnitude of the testing site and the scope of work that would be required to make it happen.”Jennifer Goldman, DO, MBA
Medical Director, Memorial Primary Car

Memorial Moves to Protect Vulnerable Nursing Home Residents

Randy Katz, DO, Medical Director, Emergency Services, and Judy Frum, Chief Operating Officer, Memorial Regional Hospital, are no strangers to nursing home emergencies.
In September 2017, they and a team of Memorial Regional Hospital staff rushed to help residents at a neighborhood nursing home after Hurricane Irma knocked the power out. Twelve elderly patients died from heat exposure, with more than 100 others surviving after treatment by Memorial Healthcare System hospitals.
That experience inspired their proactive response in the COVID‑19 pandemic. Learning from mitigation protocols in place at Memorial Healthcare System’s own nursing home, Memorial Manor, they established an outreach plan offering those same services to nearly 60 unaffiliated facilities throughout south Broward County.
“This type of outreach is personal to us,” Ms. Frum said.
Memorial partnered with the Hollywood Fire Rescue Strike Force to develop the plan, which included:
- Education and links to resources like PPE, and setting up isolation units where necessary
- Limiting staff assignments to avoid interactions between caregivers
- Performing temperature checks at the start and end of all shifts
- Scrupulously disinfecting all facilities, and suspending visiting hours
- With the help of the Florida Department of Health and the Agency for Health Care Administration, testing all nursing home residents and staff every two weeks
- Transferring positive symptomatic patients to Memorial facilities for treatment
- Removing positive-testing staff members from the nursing homes, with two negative tests required to return to work
“With almost 60 facilities, our initiative was no small task. While it would have been easier to have not pursued such a high level of proactive outreach, that wasn’t an option.”Judy L. Frum, RRT, BSN, MBA
Chief Operating Officer, Memorial Regional Hospital
The initiative quickly paid dividends, as it gave Memorial opportunities to oversee virus containment in facilities that didn’t have the expertise to manage such emergency preparedness strategies, Dr. Katz said.
“Proactively attending to situations before they become a crisis can be the difference between life and death,” he added.
“It was impossible not to think of those horrible days after Hurricane Irma when reports first began to surface about what would become a worldwide pandemic. We knew that making our Irma response proactive and scaling it for a much larger audience would require bigger-picture thinking.”Randy Katz, MD
Medical Director, Emergency Services

When COVID‑19 Arrived, Donors Stepped Up


The community’s generosity continued as the coronavirus pandemic made itself felt. A $100,000 contribution from a local major donor established a COVID fund at Memorial Foundation to support the healthcare system’s efforts in fighting the disease.
Memorial Foundation used part of the gift to pay for hotel rooms for clinical employees who wanted to care for patients without exposing their own loved ones to the virus. For one employee, critical care nurse Leah Curtis, the arrangement helped give her peace of mind as she worked long weeks in COVID units at Memorial Hospital Pembroke. “We’ve all got our roles,” she said as she visited her sons from a safe distance on Mother’s Day – her 49th day away from them. “We do what we’ve got to do.”
Additionally, Memorial Foundation set up an Employee Relief Fund to assist Memorial employees who were experiencing financial hardship due to the pandemic. Employees could apply for funding assistance for housing, food, utility bills and medical bills.
On-site, the Foundation team helped facilitate the delivery of nearly 25,000 donated meals to feed Memorial employees, including those caring for COVID patients. One organization alone delivered 3,500 meals to employees who were working at the height of the pandemic in the spring.
“People would just show up, not only with food but also with PPE,” Senior Vice President and Chief Development Officer Kevin Janser said. “The outpouring of support for Memorial and our frontline employees was just incredible.”


“People would just show up, not only with food but also with PPE. The outpouring of support for Memorial and our frontline employees was just incredible.”Kevin R. Janser
Senior Vice President and Chief Development Officer, Memorial Healthcare System

A Quick Pivot to Reach the Community
Memorial Healthcare System’s Community Relations Department had notched another year of impressive outreach to the community in 2020, holding a wide array of educational programs, speakers bureau engagements, health fairs, corporate employee wellness events and school-based programs, all of which help Community Relations put Memorial’s mission – to heal the body, mind and spirit of those we touch – into concrete action.
And then COVID‑19 arrived. Like many others in the Memorial system, the Community Relations team immediately made a change.
“We pivoted our services in the last quarter to take the majority of them online,” said Milin Espino, Administrative Director, Community Relations. “About 80 percent of them went virtual, and we also added special programming to address the new challenges of the pandemic.”
Programs that moved online or were created in response to COVID included:
- Safety and Injury Prevention – Virtual classes that helped parents address safety issues with their kids at home, such as poison and drowning prevention, the basics of CPR, the Teddy Bear Clinic, and how-to’s on correctly installing car seats
- Parenting Through a Pandemic – In partnership with Gilda’s Club, online advice about effective communication with children during COVID and how to convey a sense of safety
- Virtual Speakers Bureau – Lectures by physicians and others offering education on cancer, stroke and other conditions, and how they were being affected by the coronavirus
- Elevated Community Partners Communication – Stepped up video- and message-sharing with important community leaders and organizations on a variety of COVID-specific topics to keep the community safe
“The COVID video from Community Relations was perfectly timed for us! With 36 teenagers who are all paranoid that every sneeze is the coronavirus, we will definitely be using this in our Children’s Harbor homes. Thanks so much for sharing.”Tiffani Dhooge
President and CEO, Children’s Harbor
By the end of the fiscal year, Community Relations had staged 494 activities – with nearly 70 in the last quarter alone – reaching 296,031 participants. In addition, they sponsored more than 100 virtual events on topics that covered community needs during the pandemic. “We’re proud that we were able to give our community the answers they needed to care for themselves and their families in the pandemic,” Ms. Espino said.

*By the end of FY 2020

Prior to COVID, Community Relations had created a number of additional school-based programs, including classes on vaping, cyberbullying, violence in teen dating, the dangers of human trafficking, and other current topics of concern to the community. Those and other programs will continue in a combination of in-person and virtual outreach once the coronavirus emergency eases.
“Social events will probably come back slowly, so we can do a hybrid of sorts – offering in-person as well as online opportunities,” Ms. Espino said. “Our transition online when the pandemic hit was not only seamless but also well-received, so we’ll continue to develop innovative ways to reach our community.”

Community Services Responds to COVID‑19

On Thursday, March 12, the coronavirus pandemic had reached enough of a peak that Memorial’s Community and Youth Services team came to a realization: The way they served the people of Broward County would have to change.
By the following day, all 115 staffers had laptops, cellphones and hotspots – and the entire department transitioned to a new service model, one that coupled virtual assistance with safe property visits to fulfill critical community needs.
Newly reconfigured services included:
- Making diaper drops to new moms – at a safe distance
- Conducting counseling for new moms and at-risk families remotely, instead of in person
- Distributing repurposed laptops to students learning at home – a total of 470 for the year in a partnership with the South Florida Digital Alliance
- Helping teens complete their driver’s ed training and providing them with after-school life skills training, both online
- Teaching foster kids how to cook and how to complete the 2020 census – all via phones, computers and tablets
Community Health Services Helps Stock the Pantry
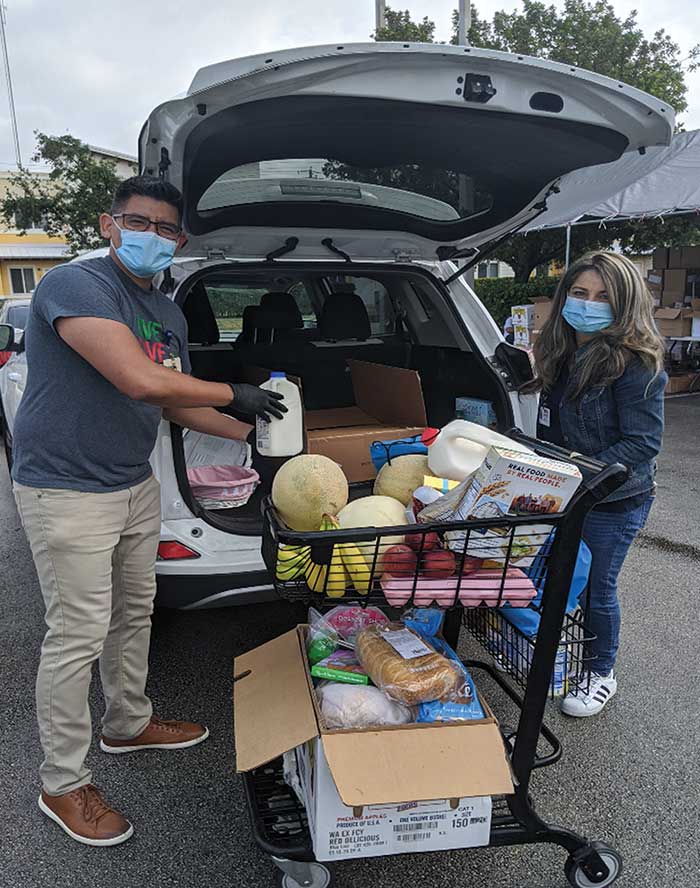
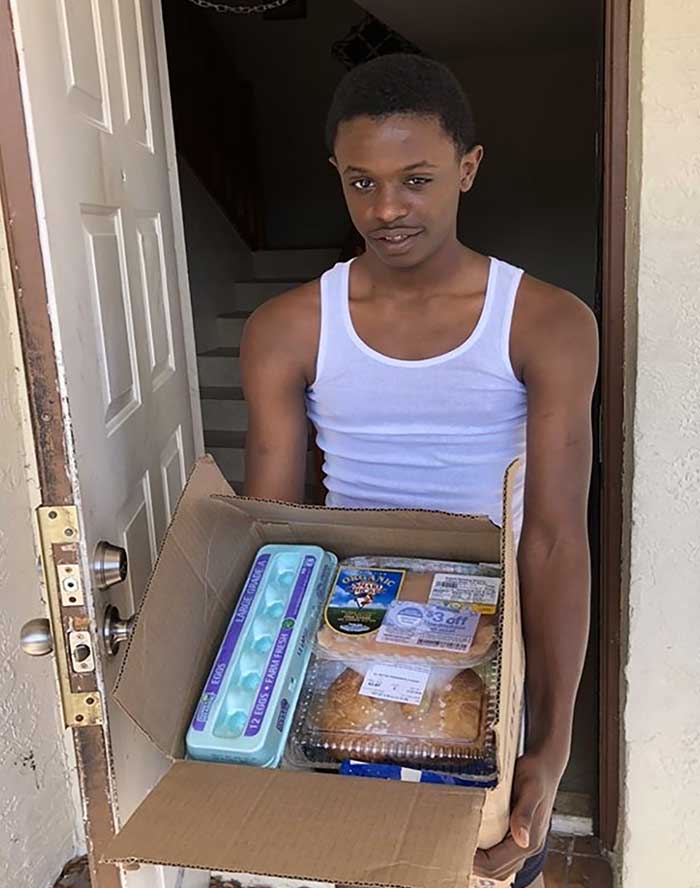
As Broward families went on employment hiatus or lost jobs, Memorial stepped in to help put food on their tables.
In support of the food bank at the Community Enhancement Center – which beefed up its food distribution in response to the pandemic – Memorial sent a dozen Community and Youth Services volunteers to the Center every Wednesday and Friday to deliver food to families in need.
“The program serves everyone from the cradle to the rocking chair – new moms, families, seniors,” said Tim Curtin, Executive Director, Community and Youth Services. “They all have different needs, but 80 percent of them have experienced job loss in their households due to the pandemic.”
From the beginning of March to mid-May, Memorial and its community partners served 675 individual families, delivering more than one and a half tons of food to approximately 150 homes per week, said Mr. Curtin.


“ALLIES Unlocked” Gets Seniors Tech-Savvy

Seniors enrolled in Memorial’s ALLIES program (Adults Living Life Independently, Educated and Safe) had a jump-start on the coronavirus: In December, Memorial paired high school students on their winter break with ALLIES participants who wanted to learn how to use their smartphones.
“The goal was to give our ALLIES participants confidence with their mobile devices,” Mr. Curtin said. “And then a few months later, boom! – they have to use those skills.”
Once the pandemic hit, the ALLIES program converted to virtual activities, serving more than 100 seniors by hosting bingo games and sing-alongs on Zoom, and connecting them to fitness classes on YouTube via their smartphones.
“The last thing our ALLIES participants want to lose is their independence, and we helped make sure that the only isolation they experienced was physical,” Mr. Curtin said.
“Our department is a strong and dedicated team. Working closely with each other and with our community partners, we were able to quickly switch gears in our service delivery when the coronavirus struck.”Tim Curtin
Executive Director, Community and Youth Services

The Office of Human Research Takes Action on COVID

Remdesivir Trials Help Speed Recovery of Some Memorial COVID Patients
Memorial’s Office of Human Research quickly joined the battle against COVID‑19 when it was selected to participate in the trial of the antiviral drug Remdesivir. A product of Gilead Sciences, Remdesivir had emerged in the first weeks of the pandemic as a potential anti-viral treatment for COVID‑19-related respiratory failure. Gilead and the National Institutes of Health supported the trials, which researchers across the country hurried to join as soon as they were opened.
After receiving permission to participate, Memorial researchers opened an Expanded Access Protocol at Memorial Regional Hospital and enrolled nine patients. At the time, Memorial was the only South Florida provider participating in the study, and one of only three in the state. The drug has been shown to lead to reduced recovery time in some patients, including a 66-year-old man at Memorial who improved enough to be removed from his ventilator just five days after his first dose.
As a result of its participation in the trials, Memorial received a supply of Remdesivir for use on an emergency basis throughout the system. Remdesivir is now given as standard of care to those patients who meet criteria for receiving the drug.
After starting with just 40 patients in April, Memorial has completed more than 1,000 convalescent plasma transfusions to date, making it one of the largest users of the treatment in the United States.
Leading in Convalescent Plasma Research
Memorial’s research team moved promptly to register for the FDA’s national Convalescent Plasma Expanded Access Program in early April.
In the Mayo Clinic-led study, blood plasma collected from individuals who have recovered from COVID‑19 is transfused to current COVID patients. Transfused donor plasma may help patients recover more quickly thanks to antibodies in the plasma that can attack the virus.
Memorial partnered with OneBlood laboratory for the plasma collection, which required close teamwork among frontline physicians, nurses, medical residents, the Office of Human Research and the blood bank. It also launched a coordinated communications campaign asking patients who had recovered from the coronavirus to become donors.
“You can imagine the logistics of all this,” said Candice Sareli, MD, Chief Medical Research Officer. “It was a huge, collaborative effort that we had to ramp up very quickly.”
To support the study, Memorial’s researchers created a database of COVID-positive patients who had been treated at Memorial and who could serve as possible donors of convalescent plasma. “This database will be very important for our retrospective research on COVID‑19,” Dr. Sareli said. “We’ll be able to see how the disease affected our community, what therapies worked, and what disparities existed in our population.”
“We have been so privileged to be at the forefront of these important COVID research studies because they’re taking place at a time when people have a true appreciation that science is important – that science really matters.”Candice Sareli, MD
Chief Medical Research Officer, Memorial Office of Human Research

Financial Report: The Effects of the Coronavirus Pandemic
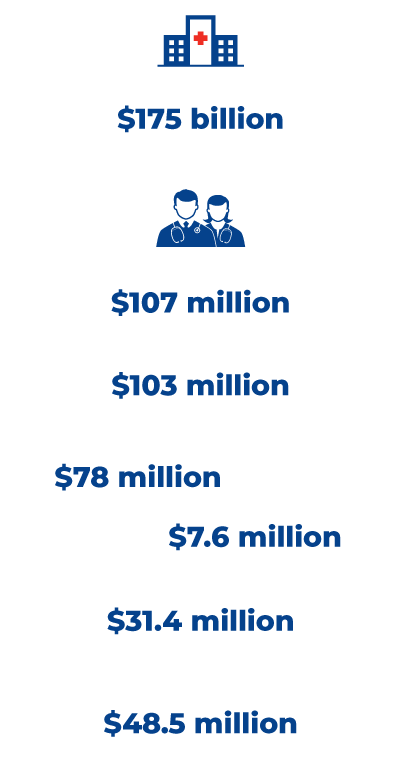
After the coronavirus struck the US, Congress passed the CARES Act Provider Relief Fund – and began distributing $175 billion nationwide to hospitals and healthcare providers experiencing substantial revenue losses from the pandemic.
“Safety-net hospital systems like Memorial have to be there for patients and families when they need us, even in a pandemic,” said David Smith, Senior Vice President and Chief Financial Officer. “The CARES Act has helped Memorial do that.”
The Act provided relief to healthcare providers in several ways. One was via expedited reimbursements from Medicare, to make up for the disruption that the pandemic was expected to cause in claims submissions and processing. Memorial Healthcare System received approximately $107 million in accelerated refundable Medicare payments.
Another avenue was the direct distribution of billions in federal funds. CARES Act payments – plus others that the government made to safety-net providers like Memorial that operate nursing homes and/or that receive Medicaid reimbursement – have so far brought Memorial a total of approximately $187.5 million in COVID‑19 distributions.
Memorial had originally budgeted nearly $103 million in operating income for FY2020. The pandemic resulted in the system recording approximately $78 million in volume-related revenue losses, plus a $7.6 million increase in expenses for items such as personal protective equipment, outdoor tents for COVID triage at each of the hospitals, and differentials paid to employees working COVID shifts.
Memorial was able to offset some of these losses with $31.4 million in reduced expenses due to lower volumes and effective cost management strategies. By the end of the fiscal year, excluding any additional revenue from the CARES Act or other sources, Memorial reflected actual operating income for 2020 at $48.5 million.
“While Memorial was fortunately in a strong financial position to begin with, our final numbers for FY2020 showed that we took a substantial hit – and we will not have a short road to recovery,” Mr. Smith said.
But although the pandemic effectively shut down Memorial’s outpatient operations – with outpatient surgeries and visits down by 82 percent and 70 percent, respectively, from April 2019 – the system’s service to community in need was uninterrupted.
“With the COVID and emergency care we provided, the thousands of telehealth visits we conducted, and our community education initiatives, Memorial continued to meet the needs of patients and families seeking care in an extraordinary time,” Mr. Smith said.
“With the COVID and emergency care we provided, the thousands of telehealth visits we conducted, and our community education initiatives, Memorial continued to meet the needs of patients and families seeking care in an extraordinary time.”David Smith, FACHE
Senior Vice President and Chief Financial Officer

Life After COVID: Memorial Rehabilitation Institute Leads the Way


With its Medically Complex Rehabilitation Unit and the expertise of its specialty-trained physicians, therapists and nurses, Memorial Rehabilitation Institute at Memorial Regional Hospital South – already one of the busiest and most comprehensive rehabilitation providers in South Florida – quickly proved itself the caregiver of choice for South Florida patients navigating their COVID recoveries.
“We found our role and purpose in the pandemic,” said Doug Zaren, Administrator and Chief Executive Officer, Memorial Regional Hospital South.
Memorial took some crucial first steps. First, it reserved the Medically Complex unit – featuring specialized equipment and technologies to help patients recover from complex conditions like acute respiratory distress – solely for coronavirus patients. Second, it educated its staff – including 11 physical medicine and rehabilitation physicians, therapists, nurses and other clinicians – exclusively on COVID recovery procedures. The institute marshaled all its resources to help patients who began arriving from both within Memorial and from other area hospitals. Many of them had spent weeks on ventilators.
“We truly became known as the COVID-recovery acute rehab program in South Florida,” Mr. Zaren said.
The nimble response was a demonstration of Memorial’s culture in action, Mr. Zaren believes.
“We have always been about quality, safety and service – and also about the ability to adjust when we need to,” he said. “As a public healthcare system, we’re amazingly agile.”
Stepping Up to Meet the Challenge of Changing Realities
The team at Memorial Rehabilitation Institute needed to figure out two things: How to respond to the initial impact of COVID? And how to help patients from other hospitals recover?
Early in the pandemic, Memorial paused its visitor policy. At Memorial Rehabilitation Institute, this was a special complication – because a large part of successful rehabilitation involves caregiver training, said Dawn Broksch, PT, DPT, MAOM, FACHE, Administrative Director, Rehabilitation Services.
“With no family members or visitors allowed, we had to figure out how to do that training in a different format instead of face-to-face and on-site at the hospital,” Ms. Broksch said. “We used technology applications via smartphones and tablets in order to provide the most comprehensive training possible.”
Around the same time, Memorial Rehabilitation Institute moved to accept transfers of recovering COVID patients from other hospitals. By late April, to maximize efficiency, Memorial Regional Hospital South had stopped admitting COVID patients to its ER, transferring the COVID patients they had to other Memorial acute-care facilities and focusing exclusively on recovery.
The institute coordinated protocols with the rest of the Memorial system, establishing testing requirements and other processes. Then, for each COVID-recovering patient, they developed a plan of care based on the patient’s needs post-admission – and on what it would take to get the patient home.
“Most of these patients had been in the hospital for 30-plus days by the time they came to us,” said Shelly Delfin, APRN, MSN and Chief Nursing Officer, Memorial Regional Hospital South. “They were really itching to go home. They worked so hard to do what they needed to do to get there.”
Despite the restrictions of COVID, the rehab team involved families as much as possible, wheeling patients to the hospital’s solarium so that their loved ones, standing outside, could see them through the windows. “We did a lot of that for these patients because we recognized how isolating so much of this care was for our patients,” said Ms. Broksch.
The additional responsibilities required the rehabilitation staff to work together as a team, creatively and collaboratively. No one had a blueprint to work from, either.
“There was no playbook for this,” Ms. Delfin said. We just kept moving and made sure that we were doing what we had to do for our patients, their families, the healthcare system and our community.”
One silver lining: the chance to institute practices that uplifted the staff as well as patients, like prayer circles and resilience breaks, which may outlast the COVID pandemic itself.
“When COVID is over, we will apply a lot of these lessons to our ‘regular’ healthcare,” Ms. Delfin said. “There were a lot of good things that happened in this journey.”
“Memorial Rehabilitation Institute at Memorial Regional Hospital South truly became known as the COVID-recovery acute rehab program in South Florida.”Doug Zaren, FACHE
Administrator and Chief Executive Officer, Memorial Regional Hospital South
Switching Up the Home Health Model

One sure sign that the coronavirus pandemic had hit Memorial Home Health Services: Patients became nervous about having visitors. How do you provide home health if you can’t be in the home?
Home Health quickly moved to reassess its scheduling, prioritizing patients who needed services only healthcare professionals could provide – such as wound care, IVs and injections – and pulling back on visits for services like bathing and feeding, for which family members could step in.
“Over time, we figured it out,” said Meryl Comiter, Administrator, Home Health. “We tried to get really creative. For example, we determined patient by patient whether we could do a home visit for, say, an evaluation and then conduct the rest of the visits virtually.” Memorial’s was the first EPIC home health agency to offer virtual visits for both therapy and nursing, Ms. Comiter added.
Like so much else that the pandemic response demanded, flexibility was the key to success. With home visits curtailed, a third of Home Health’s 86 team members moved, like their co-workers across the system, to other assignments within Memorial – working as screeners, for example, or sewing face masks.
These transitions ran more smoothly than they might have thanks to Home Health’s status as a member of the Memorial system, Ms. Comiter noted.
“Because we’re part of an integrated healthcare system that believes in safety first, we had PPE that other home health agencies didn’t,” she said. “Also, as part of a post-acute-care continuum, we could more easily adapt to challenges and cover all contingencies. And our COVID experience with virtual visits has given us the foundation to keep improving our communications with patients and families once the pandemic is over.”



















