This year, 17,451 patients received cardiac procedures at Memorial, including:
;?>)
MOVING MEDICINE FORWARD





The Difference We Make in the Lives of Patients and Families Is Our Story
Memorial Cardiac and Vascular Institute continued to demonstrate this year that it qualifies as a comprehensive resource for TotalHeart care, having received national recognition for excellence in specialized and coordinated cardiovascular care.
The institute once again earned the highest rating from the Society of Thoracic Surgeons (STS), receiving three-star ratings in coronary bypass grafting (CABG), aortic valve replacement and repair (AVR) and isolated mitral valve replacement/repair (MVRR) for the reporting period July 2017 to June 2018. The three-star rating places Memorial among the most elite cardiac programs in the US.
Memorial also received the American College of Cardiology’s highest rating for outcomes related to diagnostic cardiac catheterization and percutaneous coronary interventions (PCI) at both Memorial Regional Hospital and Memorial Hospital West.
Watchman Offers Long-Term Solutions
This past year, Memorial Cardiac and Vascular Institute began implantation of the Watchman left atrial appendage closure device in patients with atrial fibrillation not caused by a heart valve problem. Implanted via a minimally invasive procedure, the Watchman is a small permanent device that helps reduce the risk of stroke in patients who are at too-high risk for ongoing therapy with anti-coagulants (blood thinners).
Interventional procedures such as TAVR, Watchman and MitraClip – all used to treat heart disease – require a multidisciplinary team approach. Experts in cardiac imaging, cardiac surgery, and both general and interventional cardiology review each case in conference, in order to ensure we offer the best treatment options with optimal outcomes.
Quick TotalHeart Facts
- Memorial Cardiac and Vascular Institute uses the radial artery (wrist) versus the groin approach to perform more than 70 percent of all cardiac catheterizations and percutaneous coronary interventions
- The national average of radial access is 35 percent
- The radial approach reduces bleeding and discomfort, and allows patients to be discharged home from the hospital sooner, with a lower incidence of complications
New CVICU, ECMO Offer Leading Technology, Expertise
Memorial Cardiac and Vascular Institute opened its new, state-of-the-art 19-bed cardiovascular intensive care unit (CVICU) at Memorial Regional Hospital. This unit and its dedicated staff of experts provide leading-edge cardiovascular care to a wide range of patients.
“We’re a comprehensive team – physicians, intensivists, nurses, respiratory therapists, pharmacists, nutritionists – that is also very specialized,” said Lance Cohen, MD, FCCP, Medical Director, Cardiovascular Intensive Care Unit. “Cardiac care is all we do, and when you only do one thing, you become very good at it.”
One technology often used in the CVICU is extracorporeal membrane oxygenation, or ECMO – an advanced form of mechanical circulatory support provided at the bedside, similar to a heart-lung machine. With ECMO, a pumping machine temporarily puts oxygen into the blood, removes carbon dioxide and provides blood flow in critically ill patients with all causes of heart and lung failure.
“The overall depth of our services means that our multidisciplinary ECMO team can address every issue that these complex patients may have,” said I-wen Wang, MD, PhD, FACS. “Our team is now performing this surgical procedure at bedside throughout Memorial, offering critically ill patients immediate 24/7 access.”
Memorial Cardiac and Vascular Institute remains the only provider in South Florida offering mobile ECMO services. “We provide this bedside ECMO access to other hospitals in South Florida that do not have this service, providing safe hospital-to-hospital transfers under the care and supervision of our ECMO transport team,” said Dr. Wang.
“At Memorial Cardiac and Vascular Institute, we provide definitive, comprehensive services to our patients. They don’t have to travel to other institutions – those providers send their patients to us, and come to us for advance training. With our quality ratings and outcomes, unparalleled expertise and the latest in technology, cardiac patients and their families know that our excellence is their road to recovery.”Michele Slane
Vice President, Cardiac and Vascular Services, Memorial Cardiac and Vascular Institute
Memorial Cardiac and Vascular Institute has performed its 100th ECMO since the program was established in 2015. A critically ill trauma patient – having suffered two cardiac arrests and not oxygenating well despite being on a ventilator – was placed on ECMO in the Trauma Surgical ICU and then transferred to the CVICU. “It truly defines Memorial’s culture that the collaborative effort between the surgical intensive care unit team and the CVICU team was seamless and got the job done,” said Clinical Manager Valerie Soto, RN, CM, TCRN.
With Memorial Cardiac and Vascular Institute, Peter Gets Another Shot
Peter woke up during the night, unable to get comfortable. With his heart racing, he and his wife drove to the Memorial Regional Hospital Emergency Room.
During an MRI, Peter went into cardiac arrest.
“He coded on the MRI table,” said his wife, Janice. “Important decisions had to be made very quickly.”
Priyanka Gosain, MD, an advanced heart failure and transplant cardiologist at Memorial Cardiac and Vascular Institute, treated Peter. He was placed on extracorporeal membrane oxygenation (ECMO), a mechanical process to take over the function of his heart and lungs, while the heart received the medicine it needed.
Peter’s condition was grave, and a transplant was initially considered. Instead, he was able to be weaned off the mechanical support and he improved tremendously.
“Because of the great teamwork at Memorial and by Dr. Gosain, no transplant is needed,” Peter said. “I still have my own heart. I have another shot.”
Making Patients Stronger Against Cancer
Memorial Cancer Institute continues to be a leader in the fight against cancer with innovative treatments and testing to give cancer patients an important gift: time. Lung cancer is just one example.
“Thanks to the precision medicine we practice, our lung cancer patients’ survival rates can increase to five or even more years instead of the average rate of one year,” said Luis E. Raez, MD, Chief of Hematology and Oncology and Medical Director, Memorial Cancer Institute. “That additional time can make all the difference, because it helps bring genetic discoveries and new drugs that are not available elsewhere in Florida.”
Moffitt Partnership Brings New Treatments, Benefits
Cancer patients coping with the blood and bone cancers leukemia, lymphoma and myeloma are benefiting from Memorial’s clinical partnership with Moffitt Cancer Center – a National Cancer Institute-designated Comprehensive Cancer Center in Florida which is recognized as one of the 10 best cancer centers in the US.
Moffitt Malignant Hematology & Cellular Therapy at Memorial Healthcare System provided 74 patients with bone marrow/stem cell transplants at Memorial Hospital West this year, and opened its first clinical trial for patients with myelodysplastic syndrome (MDS) – the first of many studies that will be offered.
“We’ve doubled the number of transplants that we provided in our first year of the program, and will continue to bring novel therapies so that cancer patients will no longer have to travel elsewhere to get their care,” said Hugo Fernandez, MD, Chair and Medical Director, Moffitt Malignant Hematology and Cellular Therapy.
Memorial will begin a clinical trial for CAR-T cellular therapy in multiple myeloma, in which patients’ immune cells are enlisted to attack the cancer cells. “Immunotherapy is the future of cancer care,” Dr. Fernandez said.
Therapies Target Solid Tumors
Molecular-based innovations in cancer treatment have brought particular benefits to patients with solid tumors of the lung, head and neck. Memorial Cancer Institute is utilizing such targeted therapies to treat genomic alterations that are responsible for the growth of such cancers – with better response rates and less toxicity than customary chemotherapy and radiation combinations.
“Treatments for these tumors have traditionally been very taxing,” said Brian Hunis, MD, Associate Medical Director, Memorial Cancer Institute, and Medical Director, Head and Neck Cancer Program. “Targeted, de-intensified therapy allows us to use lesser doses of radiation with either no chemo or a less-intensive schedule of chemo.”
The new therapies help patients regain their strength and their ability to resume normal activities more quickly, Dr. Hunis said. “Our goals are to keep elevating our level of care and to expand our access to research – all while maintaining the close, one-on-one partnership we have with our patients.”
Genomics Result in Earlier Treatments
Since December 2018, Memorial Cancer Institute’s genomic testing lab has provided patients with faster results that help point them toward the right treatments in less time. “We often can get results in fewer than 10 days after diagnosis,” said clinical pathologist Artur Rangel, MD, PhD. “That means less anxiety for the patient and faster decision making on what treatments to go for.”
The lab began with genomic testing for solid tumors, such as for the liver or the lung, and soon will expand the program to include genomic testing for blood malignancies like lymphoma.
Genetics Program Helps Fill in the Blanks
Genetic predisposition testing can help reveal whether a patient has the potential for developing cancer in the future. It can detect an inherited mutation in a gene that the patient was born with but unaware of. It can also provide valuable information to patients’ family members about their own risks.
Memorial Cancer Institute’s genetics program offers patients hereditary cancer testing of 30 to 60 genes to help patients make informed decisions about their cancer risks. This year, the program served an average of 60 patients per month, and is already set to surpass the number served over the entire previous year.
In addition to testing, the program works with patients on developing personal care plans, including nutrition and healthy lifestyle choices.
“Hereditary cancer genetic testing is the best available tool to give you vital genetic information about cancer risks for yourself and your family,” said Tammy Adar, certified genetic counselor and manager of the Genetic Counselor Program. “However, regardless of testing, an important step all patients must take is to know your family history, communicate with your family members, and make your doctor aware, too.”
“Targeted, de-intensified therapy allows us to use lesser doses of radiation with either no chemo or a less-intensive schedule of chemo.”Brian Hunis, MD
Associate Medical Director, Memorial Cancer Institute, and Medical Director, Head and Neck Cancer Program
Center of Excellence in Lung Cancer
For several years, the lung cancer program at Memorial Cancer Institute has been working to develop precision medicine – developing new diagnostic technologies and therapies that are different for each patient and that can bring better success. This contrasts with empiric chemotherapy, which has been the approach for decades, with little benefit to patients.
One example is Memorial Cancer Institute targeting tumors with new therapies. Over the last two years, the institute was the only provider in South Florida where the agents larotrectenib and lorlatinib were available to target the genes NTRK 1,2, 3 and ALK/ROS1 prior to their FDA approval at the end of 2018. Several patients, both from South Florida and from abroad, were treated with these new agents.
Memorial Cancer Institute also works with new diagnostic technologies in blood – “liquid biopsies” – in which genes that are responsible for cancer can be identified in blood, and tumors can be tracked during therapy, using cfDNA and cfRNA. Luis E. Raez, MD, Chief of Hematology and Oncology and Medical Director, Memorial Cancer Institute, spoke on these leading-edge studies at the 2018 World Lung Cancer Conference in Toronto. “This is an effort to track patient outcomes in real time – not needing to depend on costly imaging studies that expose patients to radiation,” Dr. Raez said.
Memorial Cancer Institute’s lung cancer program received the Lung Cancer Center of Excellence designation from the BALC Foundation in 2012, and soon after that, Lung Cancer Screening Center of Excellence designation from the Lung Cancer Alliance. Since then, Memorial Cancer Institute has taken a leadership position among 38 lung cancer centers of excellence to enhance quality of care in lung cancer. In December 2018, Dr. Raez chaired the National Center of Excellence Summit. He is leading the group working on new guidelines, presented in the World Lung Cancer Conference in 2018 and slated for review later in 2019.

Twins Beat Breast Cancer Together
Sisters Chimene and Cheryl enjoy that special bond that exists between twins, including similar life journeys. They’re both married with three kids, both teach at Miami Dade College and they’re both breast cancer survivors.
When Cheryl found a lump in her breast, she went to Memorial. She was diagnosed with Stage 2 breast cancer, and with the expert care of her Memorial cancer team, Cheryl beat back the disease. Five years later, Chimene found a lump. She had the same type of breast cancer.
“She had to go to Memorial because they were so great with me,” Cheryl said.
Memorial physicians had learned a lot from a clinical trial that Cheryl participated in.
“The research study that she did became the standard of care for what I did, five years later,” Chimene said.
Aeisha Rivers, MD, breast surgical oncologist, recalls that “if you saw one sister, you saw the other,” and their special bond made a difference in their recovery.
“Yes, we are better together for sure,” Cheryl said.
Growing and Gaining More National Recognition
Memorial Neuroscience Institute has continued to receive recognition as a leading regional medical center for complex neurological injuries and conditions – solidifying its position as an outstanding resource for patients coping with stroke, aneurysms, Parkinson’s and Alzheimer’s disease, brain and spinal tumors, epilepsy, migraines, brain vascular conditions, and more.

One example is its multidisciplinary approach to stroke. This year, Memorial Neuroscience Institute at Memorial Regional Hospital and Memorial Hospital West once again received the Get With The Guidelines Stroke Gold Plus Achievement Award, as well as Target: Stroke Honor Roll-Elite Plus designation, from the American Heart Association/American Stroke Association. This recognition pays tribute to Memorial’s ability to provide the highest level of specialized stroke care: To be eligible, hospitals must demonstrate compliance with stroke-related standards developed according to nationally recognized, research-based guidelines.
“It takes a lot of teamwork to sustain the rapid door-to-treatment times that help avoid permanent loss of mobility and functionality,” said Brijesh Mehta, MD, Medical Director, Neuro Critical Care and Acute Stroke Intervention Program. “While we’ve earned these designations at both Memorial Regional Hospital and Memorial Hospital West for years now, we still engage in ongoing quality improvement efforts, which have allowed us to maintain such a high-caliber stroke program.”
This year, those efforts included continuing education with community paramedics on the core components of effective stroke care – the importance of fast treatment, “the golden hour,” and the difference it can make to patients when they are brought to an elite stroke center like Memorial.
“Our door-to-treatment time is less than 60 minutes in 75 percent of our cases, and less than 45 minutes in at least half,” Dr. Mehta said. “Our ability to offer comprehensive stroke treatment 24 hours a day means a vastly improved experience for the patient.”
“Memorial Neuroscience Institute is a comprehensive center for the full range of complex neurological conditions. There are only a few like us in South Florida, and we are well-positioned to bring new programs, new technologies, and even more innovative programs to those we serve.”Christopher DeMassi, MD, FACS, FAANS
Chief of Neurosurgery, Medical Director, Memorial Spine Center
Memorial Neuroscience Institute at Memorial Hospital West Marks a Year of Growth

Daniel Aghion, MD, began his supervisory duties for Memorial Neuroscience Institute at Memorial Hospital West in 2018 – and he’s seen a lot of growth in just a year.
“We’ve grown about 20 percent just in surgical volume, not just in the transfer of patients but in new patients,” he said.
While neuroscience services are expanding at Memorial Hospital West, it is not at the expense of the hospital’s family-oriented atmosphere, Dr. Aghion explained.
“We have the benefit of treating patients as if they’re at a small community hospital, but with leading-edge neurological care that comes from the backing of a large academic institution and all of its resources,” he said. “It really is the best of both worlds.”
With its growth – a new bed tower, two new ORs, a neuroscience floor, and the addition of neurological rehabilitation, social work and case management services – Memorial Neuroscience Center at Memorial Hospital West is poised to be a leader in providing multidisciplinary neurological treatment in western Broward County.
“Patients are seeking centers of excellence, and that’s what we’re building,” Dr. Aghion said.
“We have the benefit of treating patients as if they’re at a small community hospital, but with leading-edge neurological care that comes from the backing of a large academic institution and all of its resources. It really is the best of both worlds.”Daniel Aghion, MD
Neurosurgeon
Epilepsy Program Receives Recertification, Is Set to Grow

Memorial Neuroscience Institute Comprehensive Epilepsy Center provides expert treatment to help patients manage epilepsy, seizures and other clinically complex neurological conditions – without having to leave South Florida.
“We’ve continued to provide patients with comprehensive epilepsy care, from their initial diagnosis to multiple treatment options – including medication, surgery and brain stimulation,” said Tarek Zakaria, MD, Medical Director, Adult Neurology Program and Epilepsy Program.
In January 2019, Memorial was recertified as a Level 4 Epilepsy Center – the highest level of recognition that the National Association of Epilepsy Centers (NAEC) can bestow – for providing advanced treatment options for epilepsy. And the institute is set to expand its options and services further: New technologies such as robotics and deep brain stimulation are planned for the coming year, and Memorial’s Graduate Medical Education program is set to welcome its first class of neurology residents in June of 2020.
“The need for neurological residents continues to grow, especially in South Florida,” Dr. Zakaria said. “It is very important that Memorial is leading the way in having well-qualified neurologists to handle this demand for high-level neurological treatment.”
“We’ve continued to provide patients with comprehensive epilepsy care, from their initial diagnosis to multiple treatment options – including medication, surgery and brain stimulation.”Terek Zakaria, MD
Medical Director, Adult Neurology Program and Epilepsy Program
Facts on Memorial Neuroscience Institute’s Stroke Program

- Is one of the few providers in Florida with a multidisciplinary team of interventional neurologists and neuroradiologists working together to provide acute stroke treatment
- Treats more than 1,500 stroke patients every year at Memorial Regional Hospital and Memorial Hospital West
- Is the only Joint Commission-certified Comprehensive Stroke Center in Broward County (at Memorial Regional Hospital)
- Has one of the highest treatment rates for brain aneurysm in Florida
- Participates in multiple randomized and controlled research studies that will help advance the treatment of stroke
Extraordinary Stroke Care at Memorial Neuroscience Institute
Heading out to dinner with her mother, Karen felt a headache coming on. After dinner, they went for coffee and that's when the headache transformed into something more ominous.
“I couldn't see on my right-hand side; I could only see left,” Karen said. “I missed the turnoff to get the coffee and decided that I better go home.”
Fortunately, Karen's neighbors stopped by the next day. They found her in bad shape, unable to even sit up, and immediately called Hallandale Beach Fire Rescue. While en route to the hospital, the paramedics contacted Memorial's stroke hotline. Based on her severe neurological impairment, a stroke alert was called.
At Memorial Regional Hospital, a CT scan of her brain revealed Karen had suffered a stroke, with a significant blockage of her carotid artery. Under the direction of Brijesh P. Mehta, MD, Medical Director, Stroke and Neurocritical Care at Memorial Neuroscience Institute, Karen underwent an emergent mechanical thrombectomy that successfully opened her artery. The procedure was performed within 60 minutes of her arrival at Memorial, often deemed the “golden hour” for acute stroke care.
“At seven days, I woke up and stretched and went, ‘Yahoo! I’m free,’” Karen said. “I was able to move everything. It was amazing. I had the best care ever, right from the get-go.”
Her stroke care team was also feeling pretty good.
“Each time we see an artery open up, it's unbelievable, the personal satisfaction that we get,” said Dr. Mehta. “There's no other feeling that can match that, in terms of a good outcome for the patient.”
Post-Acute Care Network Goes Beyond to Meet Patients’ Needs
Thanks to its full range of post-acute care services – inpatient and outpatient rehabilitation plus skilled nursing delivered by both our award-winning nursing home, Memorial Manor, and Home Health – Memorial Rehabilitation Institute has become the provider of choice for patients seeking care after a hospital stay.
This Year:
2,237 inpatient rehab admissions for patients recovering from stroke, trauma and neurological conditions
169,906 outpatient visits for occupational, physical and speech therapy
4,436 Home Health patients admitted
63,391 Home Health visits
Memorial Rehabilitation Institute is one of the busiest and most comprehensive rehab providers in South Florida.
Last year, Memorial began offering a fully comprehensive adult sports medicine program, with orthopedic surgery, primary care, rehabilitation and physical therapy specialists and cardiology all in one program.
National Recognition for Excellence in Rehabilitation
Family In Training (FIT) – For its successful emphasis on involving families with their loved ones’ rehabilitative care, the FIT program won the 2018 Sherman Award for Excellence in Patient Engagement from EngagingPatients.org. The award salutes innovative programs that help providers build meaningful and effective relationships and communication with patients and families.
The FIT program also was honored with the IHI/NPSF Lucian Leape Institute’s Medtronic Safety Culture & Technology Innovator Award, which recognizes organizations that have successfully implemented new processes in healthcare through technology and/or culture change.
In its second year, the FIT program trained 336 family members in helping patients walk, handle a wheelchair, or transfer from a bed to a chair or toilet, with only two patients experiencing a family-related fall.
Ranked the Best – Memorial Manor, which provides skilled nursing services to rehabilitation patients in the nursing home setting, was once again recognized by US News & World Report as a Best Nursing Home for 2018-2019 for its safety and personalized, high-quality care.
“Memorial Rehabilitation Institute continues to lead in post-acute rehabilitation by offering a wide range of services. No matter where rehabilitation patients are in the continuum – inpatient, outpatient, in a skilled nursing facility or at home – Memorial Rehabilitation helps get them back to their families, their jobs and their lives.”Alan K. Novick, MD
Medical Director, Memorial Rehabilitation Institute
Adaptive Sports Play Leading Role in Rehabilitation
Memorial Rehabilitation Institute hosted more than 200 participants at its fifth annual Adaptive Sports & Recreation Expo this spring in Markham Park. Patients, their families and members of the community took part in a broad array of adaptive sports activities, including wheelchair basketball, fishing, sailing, scuba diving, hand cycling and water skiing.
“Memorial created the Adaptive Sports Expo five years ago to help rehabilitation patients realize new goals and enjoy the freedom of physical activity,” said Ray Shipman, Director of Business Development, Sports Medicine and Adaptive Sports. “The program is growing because it appeals to a population of athletes who refuse to let their disabilities or injuries define them – which is inspiring to the rest of us.”
Mr. Shipman also launched the Adaptive Fitness Fridays, in which rehabilitation patients and members of the community participate in weekly group workouts and fitness training.




For kids wanting to play adaptive sports, Memorial Rehabilitation Institute partnered in June 2017 with Dynamic Orthopedics to form the Fort Lauderdale Junior Sharks, part of the successful Fort Lauderdale Sharks adult wheelchair basketball team. This year, the Junior Sharks – children age six to 13 coping with conditions that range from cerebral palsy to amputations – participated in their first wheelchair basketball tournament with support from Joe DiMaggio Children’s Hospital Foundation, which contributed three practice chairs to the team.
“The Junior Sharks program gives kids a group they can belong to, where they can learn social skills and the value of teamwork,” said Ali Harrington, Inpatient Therapy Supervisor, Memorial Rehabilitation Institute. “They always come to practice with their game faces on – they strive to be such good players, their disabilities just fall away.”


Graduate Medical Education Launches, Readies for More Growth
Memorial Rehabilitation Institute launched its Graduate Medical Education program in July 2018, welcoming its inaugural class of four residents in Physical Medicine and Rehabilitation (PM&R). After spending the first year in internal medicine, the residents begin three years of intensive training in physiatry, working with patients to regain and/or maximize their functional abilities and enhance their quality of life.
Coming soon: A neuro-residency program in partnership with Nova Southeastern University, to train the physical therapists of tomorrow in a patient- and family-centered care environment.
Moffitt-Memorial Partnership Essential to Cedric’s Recovery
Cedric was diagnosed with acute leukemia after being referred to Memorial. “It was a shocker,” he said. “I’m 40 years old and I have small children.”
During leukemia treatments, Cedric developed severe bleeding complications in his brain and body. For chemotherapy to continue he was placed in a coma-like state for three months.
Emerging gradually from the coma, extremely debilitated and with very little strength, Cedric worked intensively with Memorial’s physical, occupational and speech therapists to regain walking and motor skills.
Memorial physicians had learned a lot from a clinical trial that Cheryl participated in.
“For patients like Cedric, we work very closely with Memorial Rehabilitation Institute,” said Yehuda Deutsch, MD, hematologist-oncologist, Moffitt Malignant Hematology & Cellular Therapy at Memorial Healthcare System.
As he returned to treatment, Cedric looked forward to more activities with his kids and having the strength to drive his Mustang GT. “I definitely recommend Memorial,” he said. “They are the best team out there.”
Memorial Transplant Institute Offers Patients Lifesaving Kidney Transplants
 Adding Liver Transplantation Soon
Adding Liver Transplantation Soon
Sixty-five and counting: That’s how many kidney transplants have been performed at Memorial Transplant Institute since the kidney transplantation program launched in February 2018.
Receiving new kidneys were 60 adult and five pediatric patients – one of whom was the first to have the procedure at Joe DiMaggio Children’s Hospital. (The other transplants were performed at Memorial Regional Hospital.) And more referrals are coming every day, said Juan Arenas, MD, Chief of Memorial Transplant Institute and Surgical Director, Pediatric and Adult Surgical Kidney Transplant.
Once they’ve been referred, patients must be evaluated to determine if they meet medical criteria for transplantation, Dr. Arenas explained, with about two-thirds qualifying to be seen by the program. Of those, approximately half are listed for transplant – which means they may receive a kidney transplant when an organ becomes available.
Total Transplants*
Heart Transplants = 48 Adult 53 Pediatric
Kidney Transplants = 60 Adult 5 Pediatric
Bone Marrow Transplants = 243 Adult**
Liver Transplants = Coming Soon
*As of August 2019 **Moffitt Malignant Hematology & Cellular Therapy at Memorial Healthcare System
With that level of demand, Memorial Transplant Institute is continuing to grow. This year, a second adult transplant nephrologist, a third transplant surgeon and a third pediatric transplant nephrologist will join the current team of Dr. Arenas and Alexandru Constantinescu, MD, Tjasa Hranjec, MD, and Fernando E. Pedraza, MD. Additionally, with liver transplantation soon to be added to its services, the program is recruiting for a third adult transplant nephrologist and both an adult and pediatric transplant hepatologist.
“We have close to 80 patients listed for transplants right now, and continue to get an average of 60 to 70 referrals a month. Our total referrals since the program started are more than 1,500.”Juan Arenas, MD, FACS, MBA
Chief of Transplant Institute and Surgical Director, Pediatric and Adult Surgical Kidney Transplant
Memorial Foundation and Joe DiMaggio Children’s Hospital Foundation honored pediatric kidney transplant nephrologist Alexandru Constantinescu, MD, with its Spirit of Healing award this spring. The Circle of Friends recognized Dr. Constantinescu for his commitment to kidney health and his 16 years of dedicated service to Memorial’s pediatric patients and their families.

Memorial Transplant Institute: Kidney Transplant Changes Kyle's Life
Kyle came to Memorial after a diagnosis of end-stage kidney failure. For four years, he was receiving four-hour hemodialysis treatments, three times a week.
"When Memorial started its Transplant Institute, I wanted to look into getting on another transplant list," Kyle said.
Fernando Pedraza, MD, Medical Director, Adult Nephrology & Kidney Transplant Program, and a multidisciplinary team of specialists, took over Kyle's care, keeping their patient and his wife, Jean, informed at all times.
"Kyle's life was limited by these sequential treatments and his disease," said Dr. Pedraza.
Shortly after getting on the transplant list, an organ became available. After Kyle's transplant surgery, the kidney began working immediately.
Kyle has returned to his former employment and continues to retake control of his life.
"Since the transplant, everything is phenomenal," he said. "I'm at a good place – a place that I've longed to be for such a huge period of time."
Joe DiMaggio Children’s Hospital: Growing Up, Growing Strong
Joe DiMaggio Children’s Hospital is one of the leading pediatric hospitals in Florida, so it’s appropriate that “growth” is the theme for 2019, since the hospital is about to embark on the largest expansion in its 27-year history. Later this year, the hospital will begin construction to add four floors to the facility and double its size. The additional 156,000 square feet will enable the hospital to add more specialties and continue to provide the high level of patient- and family-centered care it has become known for.
The planned expansion includes:
- An MRI-equipped, neurointerventional suite for pediatric brain surgery
- Pediatric intermediate inpatient care
- Pediatric intensive care
- Indoor/outdoor rehabilitation gym
- A staff “playroom”/respite area
- A “one-stop,” multidisciplinary clinic where children with complex health issues will see multiple specialists during the same visit
- A heart institute operating suite with hybrid rooms and cardiac catheterization laboratories
- Cardiovascular intensive care
- Play space for patients and respite area for parents including a business center, fitness room and relaxation area
- A classroom for patients to continue their studies while in the hospital
- Classrooms and a simulation lab for medical and nursing residents and students

The project will cost approximately $170 million and is expected to take about two years to complete. To include the philanthropic community in its efforts, the hospital created the “Catch the Love” capital campaign to raise $50 million in support of the expansion.
“The capital campaign is meant to raise critical funding needed to support our expansion and also increase awareness of Joe DiMaggio Children’s Hospital, our services, and family-centered approach,” said Caitlin Beck Stella, MPH, CEO of Joe DiMaggio Children’s Hospital. “We believe in the healing power of play, that teamwork and family participation in care leads to better outcomes for children, and that quality and safety are everything. We’ve always had a strong community connection, and this campaign is helping us deepen those relationships. Love is at the center of everything we do.”
But Joe DiMaggio Children’s Hospital’s growth is not limited to the expansion project in Hollywood. A brand new, 31,000-square-foot health specialty center opened in Wellington in February, offering top-quality outpatient care to families in Palm Beach County and beyond.
Additionally, the children’s hospital received the Guardian of Excellence Award for patient satisfaction for the seventh consecutive year. A nationally recognized achievement in healthcare, the award honors organizations that have demonstrated outstanding performance in patient experience.
“It’s an honor to serve as this community’s children’s hospital. Families trust us to take care of their children at the most critical times and we’ll continue to expand and meet their needs.”Caitlin Beck Stella, MPH
Chief Executive Officer, Joe DiMaggio Children’s Hospital, and Pediatric Services, Memorial Healthcare System
Palm Beach County Welcomes New Pediatric Health Center in Wellington
Just months after opening its doors, Joe DiMaggio Children’s Health Specialty Center in Wellington is already making a strong impact in the community. The 31,000-square-foot outpatient facility is now operational, featuring outpatient surgery, imaging and rehabilitation services as well as the [U18] Sports Medicine program, which specializes in the treatment of pediatric sports-related injuries. Staffed with board-certified pediatric specialists in the areas of pulmonology, endocrinology, neurology, ENT, general surgery and orthopaedics, the center is committed to providing quality pediatric healthcare services in a compassionate and child-friendly setting.
The state-of-the-art facility, which opened in February, meets the need for high-quality pediatric healthcare in Palm Beach County. More than 3,000 patient visits had been reported by June, with a constant growth in volume.
At the core of the Joe DiMaggio Children’s Hospital mission is delivering exceptional healthcare and advanced technology close to home for children and their families. The new center is achieving just that for the Palm Beach County community, while also attracting patients from other parts of the state.
“The school days that don’t have to be disrupted, the work days that parents don’t have to take off, that’s what it means to us,” said Caitlin Beck Stella, MPH, CEO of Joe DiMaggio Children’s Hospital. “Our goal is to be where families and children need us when they need us.”
Among the future plans for the center are further growth and expansion, with the addition of other pediatric specialties based on the needs of the community. Its leaders expect it to continue filling the pediatric healthcare access gaps that have been present in the Palm Beach County community in the past.

More than 3,000 patient visits
had been reported by June 2019




Pediatric Transplant Program: Giving the Gift of Life
The pediatric transplant program at Joe DiMaggio Children’s Hospital is centered around a multidisciplinary team approach to performing lifesaving transplants and providing personalized care to children who would otherwise have no hope for survival.
Pediatric Heart Transplant
Joe DiMaggio Children’s Hospital Pediatric Heart Transplant Program is the most active program in South Florida and the only one to offer comprehensive transplant, advanced heart failure and mechanical circulatory support/VAD (ventricular assist device) services for infants, children and young adults with end-stage, acquired or congenital heart disease. The program is staffed by a knowledgeable, multidisciplinary team of specialists who offer cardiac transplantation and heart failure and cardiomyopathy diagnosis and management for infants, children and young adults. It provides patients with pediatric-to-adult transitional collaboration by a comprehensive and expert team.

“We provide services that children wouldn’t otherwise have access to,” said Maryanne Chrisant, MD, Medical Director of the Pediatric Heart Transplant Program at Joe DiMaggio Children’s Hospital. “These are lifelong medical commitments that children and families make. With our expertise at Joe DiMaggio Children’s Hospital and Memorial, South Florida residents do not have to leave the area to receive exceptional care.”
Nearly nine years after the program’s first pediatric heart transplant, a total of 53 transplants have been performed, with a 100 percent one- and three-year survival rate in pediatric patients, and more than 400 transplant outpatient visits per year. The heart failure and cardiomyopathy programs have had more than 600 visits since their inception.
The program continues to expand with the creation of a clinic at the hospital’s Health Specialty Center in Wellington and the addition of new physicians to its staff. Plans to further develop the current survivorship multidisciplinary clinic are in place to continue servicing the needs of this unique population on an outpatient basis. The clinic will include immunology, endocrinology, GI and cardiology, as well as social work and mental health with access to physical therapy and cardiac rehabilitation services.
Pediatric Kidney Transplant
As it celebrates its first year, the hospital’s pediatric kidney transplant program reports a 100 percent success rate. The program, one of a handful in the state, continues to focus on growing its team and actively carrying out a variety of outreach activities while evaluating patients for transplantation.
Team members include physicians with over 40 years of experience in pediatric transplant nephrology. The team works in conjunction with other departments to ensure that children who need to receive kidney transplants are ready to do so and that they receive the necessary follow-up testing after their transplants.
“We’re a new program, but we have the ability to deal with almost any complication,” said Alexandru Constantinescu, MD, Chief of Pediatric Nephrology at Joe DiMaggio Children’s Hospital. “The expertise is here. Anything that our renal community needs is here.”
Joe DiMaggio Children’s Hospital Department of Orthopaedic Surgery’s [U18] Sports Medicine Program: National Prominence and Continued Success
The Joe DiMaggio Children’s Hospital Department of Orthopaedic Surgery is entering its 30th year providing world-class care for multiple pediatric musculoskeletal conditions. For the sixth year, U.S. News & World Report ranked the Department of Orthopaedic Surgery at Joe DiMaggio Children’s Hospital among the top pediatric orthopaedic programs in the nation, and the highest ranked program in Florida. The program is known nationally for several pediatric services including the Spine Center, Hip Preservation Center, Limb Deformity Center and [U18] Sports Medicine, the most comprehensive and multidisciplinary pediatric and adolescent sports medicine program in the southeast. In the coming year, the department will be adding a Pediatric Hand and Upper Extremity Center.
As of April, the department is proud to bring its outstanding expertise to the new Joe DiMaggio Children’s Health Specialty Center in Wellington. “Our center in Wellington allows us to expand our existing services deep into Palm Beach County and provide that community with the highest quality of care,” said Jeremy Frank, MD, pediatric orthopaedic surgeon at Joe DiMaggio Children's Hospital.
A former elite wrestler, Dr. Frank has traveled the world as a team physician for the U.S. National Wrestling team and has been chosen as an official sports medicine physician volunteer at the U.S. Olympic Training Center in Colorado Springs, Colorado. This honor brings Dr. Frank one step closer to becoming the U.S. Olympic Wrestling Team physician for the summer Olympic games in the coming years.
Matthew Fazekas, MD, another pediatric and adolescent sports medicine physician at Joe DiMaggio Children's Hospital, serves as a consulting physician for U.S. Figure Skating and has also traveled internationally in that capacity. The Orthopaedics and Sports Medicine team from Joe DiMaggio Children’s Hospital was invited by Boston Children’s Hospital and Harvard Medical School to present lectures at the Female Athlete International Conference, a global meeting presenting strategies to prevent and treat female athletic injuries. The multidisciplinary team from Joe DiMaggio Children's Hospital included Dr. Fazekas as well as a group of physical therapists specializing in dance medicine.


Joe DiMaggio Children’s Hospital continues to recognize the importance of extending its services to the community. Its [U18] Athletic Training Program now provides athletic training services to all 29 public high schools in Broward County, which accounts for approximately 14,000 student athletes. In the last year, [U18] donated $16,000 in scholarships to Broward County scholar athletes.
“Our Department of Pediatric Orthopaedics has taken some giant steps over the last 12 months to further solidify our services and provide exceptional care to the community – locally, regionally and nationally,” said Dr. Frank. “We’ve really distinguished ourselves on a national level.”
Teen Becomes 50th Pediatric Heart Transplant Recipient
Halfway through his junior year in high school, Timothy started feeling sluggish and fatigued. He had to sleep sitting up, and it was at this point his parents brought him to the emergency room at Joe DiMaggio Children’s Hospital. An evaluation by the cardiac team revealed grim news. He needed a new heart.
On Dec. 1, 2018, Timothy received that new heart, making him the 50th transplant recipient for the pediatric heart transplant team at Joe DiMaggio Children’s Hospital. He went home a week later, just in time to spend the holidays with his family.
“It was difficult and hard for someone like me, who’d been healthy my whole life, to have to get a heart transplant,” Timothy said. “It’s amazing to have a second chance at life, and I couldn’t ask for anything else.”
Frank Scholl, MD, Surgical Director of Heart Transplantation and Chief of the Heart Institute at Joe DiMaggio Children’s Hospital, said it takes a village to help patients with end-stage heart failure.
“If it weren’t for this [pediatric heart transplant] program, many children in Broward County and South Florida would not be here,” he said.
Timothy’s aunt, Marcia, is grateful to the team and donor family, calling Timothy’s second chance at life a miracle.
“Our family believes in prayer, and to look at Timothy today compared to where he was a few months ago, we call it a miracle,” she said. “To the donor family, thank you.”
Elia is Cancer-Free after Stage 4 Wilms Tumor
Seven-year-old Elia’s stomach pains weren’t just tummy aches. She had cancer. Her kidney was engulfed by a tumor that grew dangerously close to her heart – too close to remove safely with surgery.
Surrounded and cared for by her Joe DiMaggio Children’s Hospital team, Elia received chemotherapy for several months, shrinking the tumor until it could be removed.
“At first I felt scared, but there’s friends all around Joe DiMaggio,” Elia said. “They make you feel special. It helped me.”
Her mom Melanie said seeing Elia happy made her feel more comfortable.
“They took away that extra layer of worry,” she said. “We were in the best hands possible.”
Sports Medicine Center Treats Injuries and Helps Adults Stay Active
The new Memorial Sports Medicine Center provides fully integrated, comprehensive care for active adults and athletes who want to treat sports injuries, maintain sports performance and prevent injuries.
Based at Memorial Regional Hospital South, the center serves adults of all activity levels, from college students to active seniors and weekend warriors to semi-pro and professional athletes, offering:
- Orthopaedic surgery
- Primary care sports medicine
- Sports cardiology
- Sports rehabilitation
- Sports physical therapy
Working seamlessly within Memorial Healthcare System, patients navigate from diagnosis to treatment to recovery under a unified treatment plan that is continually being discussed among team members and optimized based on the individual condition and treatment goals.
“Our aim is to provide the highest level of care to all patients who wish to perform at their personal peak for physical activity, especially after an injury,” said Daniel B. Chan, MD, Medical Director, Division of Orthopaedic Surgery and Sports Medicine.
“The benefits of maintaining an active lifestyle have been increasingly apparent and highlighted in today’s health literature and media,” said Dr. Chan. “Regardless of a person’s age or baseline condition, optimizing physical activity can always positively affect health.”
Advanced Training and Expertise
The center’s highly skilled surgeons and physicians have advanced training in sports medicine and related fields, offering:
- A conservative approach first, using medications, injections and physical therapy as needed
- Specialized physical therapy programs for athletes, dancers, first responders and joint replacement patients
- Advanced surgical techniques and minimally invasive procedures when appropriate to address all types of complex injuries and conditions
The team’s sports cardiologist can screen for underlying cardiac abnormalities, treat conditions that arise during sports participation, and help athletes return to sports after they have been diagnosed with a cardiac condition.
For patients with more significant injuries or conditions that require surgery, every orthopaedic surgeon on the team has specific fellowship training in advanced and minimally invasive techniques.
The Memorial Sports Medicine Center has already generated significant interest in the community and now serves as the official team provider for colleges and universities. The center has been selected by Broward College, Florida Memorial University and ASA College to provide medical support services and athletic trainers for their sports programs.
“Memorial Sports Medicine Center expects to forge several other relationships with academic institutions and athletic groups in the future and will continue to offer the same high level of treatment to all patients who entrust us with their care,” said Douglas A. Zaren, FACHE, Administrator and CEO, Memorial Regional Hospital South and Memorial Rehabilitation Institute, Memorial Post-Acute Care Network.
“By returning all patients to their maximum activity potential, we truly aim to fulfill Memorial Healthcare System’s mission of healing the body, mind, and spirit of those we touch.”
“Our aim is to provide the highest level of care to all patients who wish to perform at their personal peak for physical activity, especially after an injury.”Daniel B. Chan, MD
Medical Director, Division of Orthopaedic Surgery and Sports Medicine
Sports Cardiologist, Unbeatable Team Restore Baseball Pitcher’s Dream
Ryker, a college baseball pitcher with major league dreams, was devastated when he was told he shouldn’t play baseball again because of his heart condition.
Instead of giving up on his dreams, Ryker sought a second opinion from sports cardiologist Eli Friedman, MD, at Memorial Sports Medicine Center. “It changed my life tremendously,” he said.
Dr. Friedman, one of the few sports cardiologists in Florida, performed numerous, detailed tests and carefully interpreted the results.
“Testing in athletes is different than what we see in the general cardiac population,” said Dr. Friedman, who determined that Ryker’s extra heartbeats called premature ventricular contractions (PVCs) were low-risk. He discovered the PVCs went away entirely when Ryker exercised, meaning he could continue to play baseball.
A pitcher in college himself, Dr. Friedman and Ryker formed a fast friendship. “We connected pretty good,” Ryker said. “But the most important thing was I trusted him.”
“He was able to look at me as a teammate,” Dr. Friedman said. “Any time you’re on a team, you have to have faith in your teammates. Now we’re part of Team Ryker.”
Joint Replacement Center Helps Patients Keep Moving
Exceeding Expectations Results in High Patient Satisfaction
Patients seeking hip or knee replacement or minimally invasive hip surgery can obtain high-quality services at Memorial’s Joint Replacement Center at Memorial Hospital West – which since its inception has consistently ranked in the top 10 percent of joint replacement programs in the country.
“Over the last three years, we’ve continuously scored over 90 percent in a number of important metrics,” said Carl C. Eierle, MD, Medical Director, Memorial Joint Replacement Center at Memorial Hospital West. “This has translated into a 95 percent increase in our case volume since the program began.”
The team at Memorial’s Joint Replacement Center treats conditions that include hip arthritis, osteoarthritis and osteonecrosis, as well as conditions resulting from trauma.
The Joint Replacement Center team provides coordinated care in its new, 40-bed facility at Memorial Hospital West. Their services, however, go beyond expertise and leading-edge technology to a full embrace of patient-centeredness.
“We provide a 360-degree environment of care, in which everyone – from housekeeping and food service to the nurses and surgeons – has buy-in, and is fully invested in a positive experience for the patient,” Dr. Eierle said. “Everywhere patients and families turn, they meet caring individuals who approach their jobs as a team.”
This year, the center continued to score highly in:
AVERAGE
LENGTH
OF STAY
<2 days
(top 10%)
DIAGNOSABLE
COMPLICATIONS
<1%
(top 10%)
PATIENTS
DISCHARGED
DIRECTLY TO HOME
91%
OVERALL
SATISFACTION RATE
(HCAHPS)

92%
That commitment is reflected in the high satisfaction scores that the center receives, Dr. Eierle said. “It’s a bit of an intangible, but it results in something very tangible in terms of our outcomes,” he added.
And with a high percentage of patients – 95 percent – who said they would recommend the Joint Replacement Center at Memorial Hospital West to others, the multidisciplinary team there is busy.
“Patients continue to seek us out. The recommendations we receive are built on our quality of care, good outcomes and great services.”Carl C. Eierle, MD
Medical Director, Memorial Joint Replacement Center

Memorial Joint Replacement Center Helps Ernest Get Back on His Feet
Ernest, age 71, is proud of his long career in the construction industry. For 35 years, he ran the maintenance facility for Miami’s Port Authority. He managed cruise ship christenings and met a lot of high-level people, including former First Lady Rosalynn Carter. Later, he became a building inspector for Miami-Dade County.
“I’ve had an exciting life for someone who grew up in a trailer park with no education,” says Ernest, whose family moved to Miami in 1944.
Though rewarding, those 50 years of hard physical labor have taken their toll on Ernest’s body. A subsequent car accident caused further damage. He’s undergone replacement surgery for his knees, shoulders and wrists, and he has plates in his spine.
“I’ve abused my body. I’m a walking stainless steel guy,” says the retired contractor.
Ernest, a father of three, lives just around the corner from Memorial Hospital West in Pembroke Pines. It’s the facility he’s relied on for every procedure and the one he recommends to others seeking quality healthcare. Two years ago, Daniel Sheldon, MD, an orthopaedic surgeon at the Memorial Joint Replacement Center, replaced one of Ernest’s hips. More recently he performed the second operation on a damaged rotator cuff. When Ernest’s girlfriend, Rosalie, needed hip and shoulder surgery, he urged her to see Dr. Sheldon. This past July, she broke her ankle in two places. Once again, they called on the services of Dr. Sheldon and the Memorial Healthcare team.
“I recommend Memorial all the time,” says Ernest. “I’m a person who picks out people who are dedicated and good at what they do. [Dr. Sheldon] did an excellent job. I appreciate when I talk to him or see him. You build a personal relationship with him. We consider him to be one of the best physicians we’ve been to.”
Ernest has always thrived on work and physical activity, yet he hasn’t let his orthopaedic problems keep him down. He helps his neighbors with home repairs and maintenance. He’s looking forward to a new grandchild. And at least for the next four months, he’ll be busy tending Rosalie.
“I get tired now, [but] I love working,” he says.
Weight-Loss Program Grows, Offers Patients More Pathways to Good Health
Memorial’s Weight-Loss Surgery Program marked a milestone this year with the opening of its system-wide bariatric offices at 2301 North University Drive. With all members of the weight-loss team – surgeons, nutritionists, exercise physiologists and mental health professionals – located under one roof, the American College of Surgeons-accredited program offers a one-stop shop for patients wanting to move to healthier lifestyles with the help of weight-loss surgery.




“We have become one of the busiest, if not the busiest, programs in the region,” said Brett Cohen, MD, Chief, Bariatric Weight-Loss Program. “And now, with a centralized location that coordinates care across the entire healthcare system, our patients can more easily access our services – from the initial evaluation for surgery to the follow-up care that’s a critical part of a successful weight-loss outcome.”
Convenience and accessibility are key, Dr. Cohen explained, because the pathway to losing weight doesn’t end with the completion of a laparoscopic sleeve gastrectomy, a laparoscopic gastric bypass, or the placement of an adjustable gastric band. Memorial’s Weight-Loss Program provides a comprehensive follow-up treatment plan that includes nutritional guidance, counseling, links to support groups and telehealth consultations in addition to in-person visits.
“We tell patients it’s a marriage,” Dr. Cohen said. “We’ll be side by side with them because they’re making commitments to changes that will last the rest of their lives.”
That ongoing care and support is what distinguishes Memorial’s Weight-Loss Surgery Program from others, Dr. Cohen said. The program’s comprehensive, patient-directed care has helped triple the number of cases, with almost 900 patients improving their health and lifestyles every year.
“Making sure that patients are taken care of as individuals is central to the quality of care we provide,” Dr. Cohen said. “Other providers might approach weight-loss surgery as just an operation, but to us, it’s different. Being there for patients whenever they need us permeates everything we do.”
“Making sure that patients are taken care of as individuals is central to the quality of care we provide.”Brett Cohen, MD
Chief, Bariatric Weight-Loss Program
Bariatric Surgery Re-Energizes May
May wasn’t feeling good. She’d just had a cancer scare and was struggling with high blood pressure, her weight and lack of energy.
“I knew that in order for me to get better, I needed to take care of my weight and take care of myself,” she said.
Her physician at Memorial Cancer Institute suggested she meet Luciano Fiszer, MD, bariatric surgeon at Memorial Hospital West.
“He took the time to explain everything to me and how it would work and make me feel comfortable,” May said.
This multidisciplinary, patient- and family-centered approach is a hallmark of Memorial care.
Dr. Fiszer performed a sleeve gastrectomy to reduce the capacity of May’s stomach. She committed to lifestyle changes and has lost 65 pounds. May is eating healthy, exercising, has more energy and no longer has hypertension.
She’s happier and more confident, too.
“It just changed my life tremendously,” May said. “I feel fantastic.”
One Stop for Comprehensive Obstetrics Services
The 13,049 babies that have been welcomed into the world at Memorial Healthcare System in the last year says a lot about Memorial’s dedication to healthy pregnancies and deliveries. That, and the full range of obstetrical services, which we provide, make Memorial a true leader in obstetrics in South Florida.

“Memorial Healthcare System’s comprehensive obstetrics services are designed to serve all parts of our South Florida community,” says Mary Roberts, RN, Director of Nursing Administration and The Family Birthplace at Memorial Hospital West. “Our own team’s diversity is a reflection of our community’s, so whether we’re communicating verbally or in writing, or providing culturally sensitive, compassionate maternity care, the medical and nursing staff members at Memorial speak your language.”
This Year,
The Family Birthplace
welcomed 13,049 babies into the world:
5,160 at Memorial Regional Hospital
4,050 at Memorial Hospital West
3,839 at Memorial Hospital Miramar
Obstetrical and Maternity Services
At Memorial, patients and families who are expecting can benefit from:
- “One-stop” comprehensive OB care – Virtually all subspecialties are represented in the Memorial system, along with state-of-the-art diagnostic testing, so that care for medical and surgical needs can continue during pregnancy. With hospital encounters, imaging studies, lab results and other records centralized in one system, medical records are always conveniently accessible across Memorial, regardless of where care is provided
- The Family Birthplace – Expert and caring Labor & Delivery services located at Memorial Regional Hospital, Memorial Hospital West and Memorial Hospital Miramar
- Childbirth and parenting education – Baby care classes, “Bootcamp for New Dads,” classes for grandparents, siblings and nannies, “Babysitting Basics,” and more
- Breastfeeding services and support – Help provided by experienced International Certified Lactation Consultants
- Maternal-Fetal Medicine – A multidisciplinary program to care for those whose pregnancies are either high-risk or develop maternal and/or fetal complications.


Maternal-Fetal Medicine (MFM)
With maternal-fetal specialists, neonatal and pediatric subspecialists, obstetricians, anesthesiologists, and adult medical and surgical subspecialists, Memorial’s Maternal-Fetal Medicine Navigation program provides the latest advances and treatments to patients with pregnancies that are either high-risk from the beginning or that develop maternal and/or fetal complications along the way.
Last Year, the
Maternal-Fetal Medicine
program treated18 placenta accreta patients, with10 already being referred this year.
The MFM team specializes in maternal complications such as genetic disorders, heart disease, kidney failure and other pre-existing medical conditions, preterm labor, severe pre-eclampsia, abnormal placental invasion (accreta), and more. They also specialize in the care of women whose babies have congenital heart abnormalities or other anomalies, genetic disorders, and poor fetal growth, in addition to other fetal complications.
For example, the MFM program has seen an increase in its referrals for patients with placenta accreta, in which the placenta attaches itself to the wall of the uterus too deeply. Memorial Regional Hospital has the resources and expertise to effectively treat the condition as safely as possible.
Quality and Safety
In keeping with current best practices, the Family Birthplace has safely decreased the use of invasive interventions such as episiotomies during childbirth. For most deliveries between 2016 and 2019, all Family Birthplace locations fully met or showed significant progress toward meeting the Leapfrog quality standard of episiotomies in 5 percent or fewer deliveries.
Nursing Education and Training Keep OB Services on the Leading Edge

Memorial is dedicated to providing continuous training to its already highly skilled clinicians. In OB, that means providing them with:
- Advanced cardiac life support certification (ACLS) certification, with an additional component for obstetrics
- Certification from the American Academy of Pediatrics in resuscitation of the newborn
- Advanced education in key maternity services, like lactation, that new moms want and need
L&D Is Top Memorial Search for Healthcare Consumers
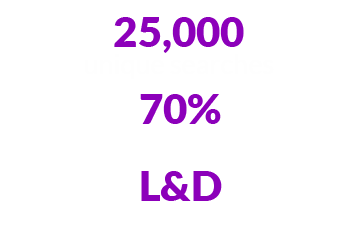
With its comprehensive OB services, it’s no wonder that Labor & Delivery has been the most frequently searched procedure on Memorial’s Transparency Tool.
The tool, which allows healthcare consumers to determine the cost of planned procedures ahead of time, has had more than 25,000 unique searches since its inception. Seventy percent of searching consumers have been women, with L&D the most popular search by procedure.
Substance Abuse Recovery Services That Are Making a Difference
Detoxification is medically managed withdrawal from drug or alcohol dependency, and most patients in Florida who are seeking such services obtain them on an outpatient basis or in a residential setting.
Memorial Medical Detoxification Program at Memorial Hospital Pembroke is different. It offers patients compassionate inpatient services to help them break the cycle of substance abuse and addiction.
Created in April 2018 in response to the opioid addiction crisis in Florida, Memorial Medical Detoxification – one of the few hospital-based addiction programs in Broward – provided addiction treatment services to its 500th patient this year, with a reported 85 percent recovery rate. Its integrated care team of therapists, case managers, counselors, psychiatrists and physicians offer treatment options for addictions to…

- Alcohol
- Benzodiazepines
- Opiates
- Heroin
- Methamphetamines
- Cocaine
…through an up-to-five-day, medically supervised withdrawal management process available 24/7 to patients who voluntarily admit themselves for treatment.
Once Memorial’s staff of trained substance abuse professionals conduct phone pre-screenings and schedule intake appointments, patients are admitted for complete medical histories and lab workups, followed by medical detoxification in a private, supervised hospital setting.
The process doesn’t stop when patients are discharged. Memorial Medical Detoxification provides customized plans of follow-up care that include referrals to support groups and other strategies designed to help prevent relapse.
Proactive, Practical Solutions to Fight the Opioid Epidemic
According to estimates by the US Department of Health & Human Services and the National Institute on Drug Abuse, more than 130 Americans die of opioid-related drug overdoses every day – and every 15 minutes, a baby is born with neonatal abstinence syndrome in the United States.
Tackling crises like these requires innovation at the local level. Memorial Healthcare System has responded with programs designed to help break the cycle of addiction – and in our emergency departments, has implemented a program to provide patients and families with the tools they need to reverse overdoses down the road and help save lives.
Since 2018,
Memorial has distributed
1,005 Narcan® kits
and has documented 25 overdose
reversals to date.
Every Memorial Emergency Department is stocked with and distributes kits of Narcan®, the brand name for the nasal medication Naloxone, which can be administered without medical training and which can reverse an opioid overdose. Since 2018, Memorial has distributed 1,005 Narcan® kits, and has documented 25 overdose reversals to date.
“That’s 25 lives saved,” said Tammy Tucker, PsyD, Associate Administrator, Memorial Regional Hospital, “and at no cost to the recipients, because Memorial distributes the kits free of charge.”
Memorial’s Multi-pronged Response to the Opioid Epidemic
The Narcan® distribution initiative is just one part of Memorial’s multi-pronged response to the opioid epidemic. We also offer:
Medication Assistance Treatment – MAT helps overdose patients who present at Memorial’s ERs by rapidly linking them with substance abuse treatment and stabilization services that will bridge them to follow-up outpatient visits. With four full-time peer specialists – patient navigators who have overcome addiction themselves – working in program, MAT has served 349 patients to date.
The SHARE Program – Individuals who can be treated on an outpatient basis receive medical detoxification services from SHARE, which offers comprehensive medical assessments and customized plans for recovery from addictions to opioids, alcohol, sedatives and other substances.
Long-Action Therapy Clinic – By providing monthly injections of Naltrexone – a long-acting drug that decreases patients’ desire to take opiates or drink alcohol – LAT helps those who are at risk for relapse overcome their desire for drugs and focus on their recovery instead.
Mothers in Recovery – This program treats addiction in pregnancy, helping expectant mothers deliver babies that are healthy and drug-free by offering obstetrical care, substance abuse treatment, case management and supportive housing. Since the program began in 2015, it has treated 128 women, with 103 live births. Ninety-four of those births were babies who were drug-free – a 91 percent success rate.
Tallahassee Goes to the Mat for MAT
Memorial’s Medication Assistance Treatment (MAT) program has received a $1 million appropriation from the state of Florida to expand its substance abuse treatment services. The funding, approved as part of the state budget and signed into law by Governor DeSantis in June, will allow Memorial to expand access to MAT for nearly 1,000 people and introduce a telehealth component to the program.
“Memorial’s approach for long-term solutions to opiate and other addictions began with Mothers in Recovery and then expanded to the general population. We were one of the first providers in the country to take the lead on this issue, and now, our data speaks for itself. It will take a long time to demonstrate the impact of our efforts, but thanks to national awareness, and government support of programs like Memorial’s, I think we’ll see a dramatic drop in addiction in the next five to 10 years.”Randy Katz, DO
Medical Director, Emergency Services, Memorial Regional Hospital


























