Moving Medicine Forward
MEMORIAL CANCER INSTITUTE

Memorial's groundbreaking partnership with Florida Atlantic University has been recognized as a Cancer Center of Excellence. (Florida Atlantic University photo)
Partnership of Excellence
The State of Florida designated Memorial Cancer Institute and Florida Atlantic University a Cancer Center of Excellence. The research partnership combines Memorial’s clinical expertise with the university’s precision research to provide patients access to clinical trials, leading to advances in cancer care and treatment.
“We have achieved this designation because we are a comprehensive center for quality research and deliver a very high level of cancer care for our patients,” said Luis E. Raez, MD, Medical Director and Chief Scientific Officer, Memorial Cancer Institute, and Co-Director for the Cancer Center of Excellence. “We have been working very hard for several years to achieve this level of care.”
The Center of Excellence designation was created to encourage preeminence in cancer care, to attract and retain the best cancer care providers, and to help Florida hospitals like Memorial be recognized nationally as a preferred destination for quality cancer care.
Florida has more than 80 oncology centers, but the Memorial-FAU partnership is one of just five designated Cancer Centers of Excellence in the state. The distinction further solidifies Memorial’s presence as a leading cancer treatment provider.
Research PACT Drives Innovation
The partnership started in November 2020, when Memorial formed a Research Partnership to Advance Clinical Trials, or Research PACT, with Florida Atlantic University.
The PACT combines the organizations’ expertise and resources in clinical research, clinical trials, basic research and translational biomedical research. Its mission is to facilitate clinical trials that lead to advances in patient care and treatment for diseases such as melanoma, lung cancer, breast cancer, pancreatic cancer and blood cancers.

The partnership with FAU began as a Research PACT.
The research affiliation also leverages the two organizations’ state-of-the-art facilities, as well as proficiency in various areas, from cancer to cardiology and biomedical engineering to big data analytics and artificial intelligence.
The scope of the agreement, limited to research and research-related education, is designed to enable clinicians and researchers from each institution to collaborate with their peers and access available resources at each partner institution.
“This is a giant step forward,” said Candice Sareli, MD, Vice President and Chief Medical Research Officer. “Through this research partnership, we will continue to expand Memorial's academic infrastructure and research portfolio and offer hope to our community and patients.”
This Research PACT is the foundational element that led to Cancer Center of Excellence designation.
Ever forward thinking, the center has big plans to develop new drugs, medical devices, software applications and other novel treatments for diseases that affect both children and adults.
Having earned the state’s endorsement, the Cancer Center of Excellence stands apart as a facility that is well-equipped, provides advanced training for personnel and moves health forward with leading cancer care.
Learn more about clinical trials at Memorial
Memorial Cancer Institute has achieved state and national recognition for leadership and innovation in cancer care. As one of only fve cancer centers in the State of Florida to merit designation as a Cancer Center of Excellence and as one of 12 nationally selected by the American Society for Clinical Oncology (ASCO) for the Patient-Centered Cancer Care Certification pilot featuring ASCO and Community Oncology Alliance (COA) to work with value-based models.”

Omar Llaguna, MD, (left) and team perform a "hot chemo" procedure.
‘Hot Chemo’ Offers Renewed Hope for Abdominal Cancer Patients
Memorial Cancer Institute has added Hyperthermic Intraperitoneal Chemotherapy — known as “hot chemo” — to its arsenal for treating abdominal cancers. The procedure has proven to be an effective alternative when all other treatment options fail.
“The prior chemo was tearing me down,” said Eddie, 51, whose cancer spread from his colon to his abdomen. “I was doing chemo every other week. When I’d get off it, I wouldn’t eat for at least three or four days. By the time I built up a little strength, I’d be right back to start chemo again. When they told me there was something else I could do, I was ecstatic.”
The treatment is the latest breakthrough in targeting gastrointestinal tumors that have spread to the lining of the abdominal cavity and surrounding areas, including the colon, appendix, rectum and ovaries.
The procedure involves flling the abdomen for 90 minutes with a chemotherapy solution heated to 104-plus degrees Fahrenheit. The aggressive technique bypasses healthy highways in the body to target the cancer cells directly and deeply, thereby reducing the side effects often seen with traditional chemotherapy, said Omar Llaguna, MD, Surgical Oncologist.
To date, Memorial Cancer Institute has treated nearly 20 patients using hot chemo, including Eddie.
“I walked out of there feeling like my old self, like there was something better than what I was going through. I believed there were better days coming,” Eddie said.

I walked out of there feeling like my old self, like there was something better than what I was going through. I believed there were better days coming.”

Telehealth Becomes Viable Cancer Care Solution During Pandemic
Memorial Cancer Institute has remained fully operational since the onset of COVID-19. Even with a shift in care delivery with the increased use of telehealth, patients undergoing cancer treatment continued to receive chemotherapy and radiation therapy or undergo surgical procedures.
Cancer patients receiving treatment require frequent medical visits, which usually are in person. Because of the pandemic, Memorial’s oncology team turned to telehealth to remain connected to patients in the safety of their own homes.
In addition, enhancements to Memorial MyChart, our patient portal and electronic health record, also helped the team to stay connected with patients throughout the pandemic, said Meredith Feinberg, MBA, FACHE, Vice President Oncology Services.
And when patients did come to the hospital or medical offces, highly enhanced safety precautions were in place at all times.
First seen as a quick fx, telehealth actually proved to be a long-term solution for creating a better model for cancer care.
“Memorial Cancer Institute is recognized as a leader of innovative cancer care delivery and continues to set high standards, demonstrating leadership in clinical research, outreach and education," said Feinberg.
Whether virtually or in person, the oncology team continued to provide Memorial-quality care and compassion.
Trouble Ahead?
While the pandemic did not impede ongoing cancer care, it did interrupt screenings and diagnoses, presenting an altogether different and frightening prospect.
“We did see a definite decline of new diagnoses over the last 18 months with COVID,” said Kim Blandon, Administrative Director of Oncology Clinical Services. "That might present a bigger problem with later disease diagnosis and progression, putting us in a more challenging position with our cancer patients since we’d have to deliver that care to a sicker, more complex patient.”
MEMORIAL CARDIAC AND VASCULAR INSTITUTE

Danielle, seen here with her son, sought care from the EP team after her smart watch alerted her to an irregular heartbeat.
EP Innovation Continues Despite Pandemic
Memorial Cardiac and Vascular Institute’s electrophysiology team has continued to enhance the patient experience despite challenges brought on by the COVID-19 pandemic.
They now send more than 90% of their patients home on the same day following their procedure and have nearly eliminated the radiation that patients experience during heart ablation procedures thanks to new technology.
Electrophysiologists diagnose and treat heart arrhythmias and other kinds of heart electrical problems. Memorial’s electrophysiology labs are some of the most active in the region — more than 1,500 procedures are performed each year.
The team began sending patients home on the same day of their procedure when it became imperative to have fewer patients remain in the hospital overnight because of the pandemic. After elective procedures were postponed due to an influx of COVID-19 patients, electrophysiology procedures were one of the first to be reinstated, Danielle, seen here with her son, partly due to the reduced overnight stays.
“We’ve had minimal readmissions and have seen great success,” said John Cogan, MD, Chief of the Electrophysiology Program at Memorial. “Patients love it, too, because they love sleeping at home.”
Memorial also opened a new, state-of-the-art electrophysiology lab where doctors are using the latest technology to deliver enhanced care.
“The room is beautiful and filled with all of the latest and greatest technology — two different mapping systems, wireless technology, headsets for communication for the team in and outside the lab and more,” Dr. Cogan said.
Memorial is a referral center for complex ablation procedures and is now performing them without fluoroscopy, which is an imaging technique that exposes patients and staff to radiation.
“The less radiation we all receive the better,” Dr. Cogan said. “We now have other technology that can replace this technique, which is safer for us all.”
Memorial specialists are also using the latest model of the WATCHMAN FLXTM Left Atrial Appendage Closure Device, which reduces the risk of stroke in those with atrial fibrillation by preventing blood clots from entering the bloodstream. The newer device can be used on more patients with different anatomies.
Beyond all the technological improvements, Dr. Cogan said the team is still what sets the program apart from others.
“You can have all the machines and technology you want, but you need the right people,” he said. “It’s a great feeling to have amazing partners who you would send your mom to in a second and knowing that the quality of care we are providing is par to none.”
each year
same day as procedure
Multispecialty Team Performs Broward’s 1st TCAR Procedure
The carotid artery in 81-year-old Reynold’s neck was nearly completely blocked with plaque, impeding the flow of blood to his brain and significantly increasing the odds that the Southwest Ranches resident would suffer a stroke.
 Reynold, Broward County's first TCAR
patient, and his wife with Sean O'Donnell, MD
Reynold, Broward County's first TCAR
patient, and his wife with Sean O'Donnell, MD
A carotid endarterectomy has traditionally been the recommended intervention, but Reynold’s age and bout with COVID-19 meant he wasn’t a realistic candidate for the surgical procedure.
The news, however, was far from bleak for Reynold, since specialists at Memorial Cardiac and Vascular Institute and Memorial Neuroscience Institute were ready to perform their first TransCarotid Artery Revascularization (TCAR), an innovative and minimally invasive procedure designed to prevent strokes in highrisk surgical patients with advanced coronary disease.
“This approach is unique in that blood flow is temporarily reversed during the procedure, ensuring any small bits of plaque that break off while the obstruction is overcome are diverted away from the brain, preventing a potential stroke,” said Sean O’Donnell, MD, Medical Director of Vascular and Endovascular Surgery at Memorial Cardiac and Vascular Institute. “We then place stents inside the artery to stabilize the remaining plaque and minimize the risk of a future stroke.”
The TCAR procedure is performed by directly accessing the carotid artery through a small incision at the neckline, just above the clavicle.
“I had a 99% blockage and was very lucky not to have had a stroke,” said Reynold, a longtime Memorial patient. “To be able to have this procedure, walk immediately after and go home the next day was a blessing.”
Memorial’s vascular and neurointerventional surgical teams collaborated on the procedure.
“The value of this multidisciplinary approach was in reviewing the clinical information and imaging studies as a team to decide the most appropriate strategy for opening up the carotid artery,” said Brijesh Mehta, MD, Medical Director of the Comprehensive Stroke Program and Neurointerventional Surgery at Memorial Neuroscience Institute.
Combating Cardiac Complications Caused by COVID-19
The heart experts at Memorial Cardiac and Vascular Institute are managing the direct and indirect impacts of the COVID-19 virus on heart health and continually evolving care for the South Florida community.
COVID-19 can cause inflammation of the heart muscle, called myocarditis, and affect the rhythm of the heart, causing conditions such as atrial fibrillation. The virus can also lead to the worsening of underlying heart conditions — such as a heart injury, blockage or damage from a previous heart attack — that people had before they got sick.
“COVID is such a challenging infection, it's going to challenge your heart,” said Ralph Levy, MD, Chief of Adult Cardiac Medical Services.
From the start of the pandemic, Memorial Cardiac and Vascular Institute mobilized specialized cardiac teams to collaborate with doctors from other specialty areas, provide comprehensive care and create protocols to help people battling COVID-19.
“We have specialized teams to take care of these patients, especially as they move into the ICUs or the cardiac intensive care unit,” he said.
The virus has also affected cardiac care in many indirect ways. Some patients experiencing symptoms of heart conditions have delayed getting treatment — especially at the start of the pandemic and during subsequent surges — because they are afraid to go to a doctor’s office or hospital.
Non-emergency heart surgeries have also been delayed periodically throughout the pandemic.
To help keep everyone safe and comfortable, cardiac teams have embraced telehealth and continue to provide care virtually and in-person.
Long-Term COVID-19 Care
Institute teams continue to care for additional COVID-19 patients as new variants of the virus arise and to monitor and treat those who have long-term symptoms.
“We recognize that some patients suffer with long-term COVID symptoms,” Levy said. “They experience a variety of lingering symptoms including brain fog, loss of appetite and taste, and some patients even have heart disease going forward that needs to be treated and addressed.”
While the pandemic has been challenging, it also brought the cardiac team and the Memorial family closer together.
“The team in a way coalesced in a very strong fashion because we have a single purpose,” Levy said. “We are here to take care of patients, while keeping us and the community safe.”
Surviving a Heart Attack After COVID-19
Larry, a 51-year-old former COVID-19 patient, returned home one day from a jog and noticed on his Apple watch that his heartbeat was irregular — spiking up to 185 and then plummeting into the 80s and then rising again.
“I knew something was wrong,” he said.
He immediately asked his wife to drive him to Memorial Regional Hospital, where an EKG showed he had a heart attack. He was rushed to the cardiac catheterization lab, so cardiac specialists could fix his heart.
“I had 100% blockage in one of my arteries, and they paged a heart surgeon to come and put a stent in,” Larry said.
While many people think of COVID-19 as a pulmonary condition, many patients have experienced heart conditions following the illness.
“COVID — as we know from studies after dealing with this for a year now — can cause dysfunction of the lining of the blood vessels called endothelium, which can increase patients’ risk of having blood clots in the heart,” said Eric Rosen, DO, Interventional Cardiologist at Memorial Regional. “We’re also seeing it in the brain causing stroke or in the lungs causing pulmonary embolism. In this case, he had a blood clot develop in the heart, which caused him to have a heart attack.”
Larry said he was shocked because he is not overweight and does not have diabetes or other pre-existing conditions that doctors have warned could be affected by COVID-19. “I don’t have any of these indicators that a lot of people would think COVID typically is going to attack,” he said.
He is grateful that the care and expertise he needed were right here. “I was actually born at Memorial Regional Hospital … and this is where I was able to turn to, to save my life 51 years later,” Larry said.

Acoustic Shockwave Technology Approved for Coronary Procedures
Memorial Cardiac and Vascular Institute is now using shockwave technology to break down calcified plaque and buildup in coronary arteries of patients, assisting in the placement of stents and the treatment of heart disease.
The Shockwave Intravascular Lithotripsy System has been used for several years for treatment in the peripheral arteries. Now, it is approved for use on the coronary arteries.
“A lot of our patients who have calcified plaques in their heart arteries are difficult to treat because the regular balloons and the regular stents don’t break the calcium,” said Juan Pastor-Cervantes, MD, Medical Director of Cardiac Catheterization at Memorial.
With this technology, physicians use acoustic waves to break up the calcium, allowing them to place and expand balloons and stents that improve blood flow. The procedure decreases the number of complications and improves outcomes for patients, Dr. Pastor-Cervantes said.
And most patients go home the same day.
“We’re looking at the best results with a minimal risk,” Dr. Pastor-Cervantes said.
Frank was the first patient to undergo the procedure at Memorial after learning that he had an 80% calcium blockage in his main artery. He wasn’t sure whether he should feel excited or concerned about being first. Now, he’s hoping the procedure becomes available for others around the country.
“This is as close to a miracle as I’ve ever been associated with,” he said. “It was a great experience, and the results were amazing.”
[With the Shockwave Intravascular Lithotripsy System] we’re looking at the best results with a minimal risk.””
MEMORIAL NEUROSCIENCE INSTITUTE

Linda, who suffered a stroke, with her son, Lance.
Young Hero Saves His Mom's Life
Time is of the essence in the world of stroke intervention. Roughly 1.9 million brain cells die every minute that passes without medical intervention. Case in point: If it hadn’t been for the quick action of 10-yearold Lance, his mother, Linda, may not have recovered as well or as fast as she did after suffering a stroke.
“Her speech was very off,” recalled Lance. “I couldn’t understand one word. She was getting up and she fell, and I ran. I got my phone and I called 911.”
The paramedics rushed Linda to Memorial, where she underwent a lifesaving procedure under the care of Norman Ajiboye, MD, Neuro-Interventional Surgeon at Memorial Neuroscience Institute.
“I activated the stroke team to come in for a thrombectomy. She also received the clot-busting medication called IV tPA. We were able to get to the clot in the brain and, within a few minutes, she was speaking better and her weakness had improved on the right side,” said Dr. Ajiboye.
Soon after the procedure, however, Linda learned she had COVID-19. While she didn’t have any symptoms, it’s likely that the virus contributed to her stroke.
“She had a defect in the inner wall of the carotid artery at the neck level. COVID has been shown to attack the blood vessel wall, and you can have an increased formation of clots and thrombus,” said Dr. Ajiboye. “That could have increased her risk of formation of clots at that deformation in the neck.”
Linda was back home with Lance three days later. Her son doesn’t call himself a hero, but he knows he was the catalyst for saving his mom’s life. Linda credits him and the Memorial stroke team’s outstanding mobilization, evaluation and treatment for saving her life.
“I’m just so happy, because I gave my son life and now he gave me my life back,” said Linda.

Christopher DeMassi, MD
Memorial Performs Its 1st Essential Tremor Procedure
In April 2021, Memorial Neuroscience Institute physicians performed the first deep brain stimulation on a patient with essential tremor.
Christopher DeMassi, MD, FACS, Chief of the institute and Chief of Neurosurgery, and Howard Kreger, MD, Neurologist, performed the surgery. The patient was a highway patrol officer who retired from the force due to her condition.
Dr. Kreger had been treating her for less than a decade when she agreed to try the procedure. Until then, it had been used at Memorial only to address the symptoms of Parkinson’s disease.
Essential tremor, or intentional tremor, is a movement disorder in which the patient experiences uncontrollable shaking while trying to perform a task. Similarly, Parkinson’s patients suffer tremors but usually only while sitting still.
Medication is initially used to treat essential tremor. However, the disease progresses to the point where medicine is no longer effective. This is when deep brain stimulation becomes a viable option.
Studies show that the procedure also could be effective in treating other drug-resistant conditions, including obsessive compulsive disorder, depression, obesity, epilepsy and substance abuse.
How It Works
Deep brain stimulation involves surgically inserting a thin wire lead attached to electrodes into the part of the brain that causes tremor. With essential tremor, that would be the thalamus. In a separate surgery, a pulse generator, or battery, is placed into the chest wall and connected to those electrodes.
Following surgery, a doctor directs the battery with a remote control to send electrical impulses to the electrodes. Ongoing stimulation regulates the abnormal impulses that cause tremor.
“There's a lot of different possible settings. You start a little conservatively, increase the voltage, then cut back and find something that's working. After that first time it's more fine-tuning. Symptoms generally improve a couple of weeks after you do the programming,” said Dr. Kreger.
Deep brain stimulation presents a lower risk of side effects than medications. It also protects the brain’s integrity better than older procedures, which burn and permanently destroy the affected tissue. Settings, frequency, amplitude and direction of the current can all be controlled with long-lasting precision.
The goal, said Dr. DeMassi, is to reduce, if not eliminate, the use of medication. Every patient is different, however, so immediate and future outcomes are unpredictable.
“The problem with both Parkinson’s and essential tremor is they slowly worsen over time. We don't have a treatment for that. We can’t slow it down. We can't stop it. All we can do is treat the symptoms, whether it's medication, exercise or deep brain stimulation,” said Dr. Kreger.
So far, the procedure has proven dramatically effective for Memorial’s first recipient. She is now able to hold a cup and a spoon without hitting her face or spilling scalding liquid on her hand.
“I was joking with the patient recently and said to her, ‘Let's go to the range. Let's get you certified again.’ She said she'd be willing to do that now,” said Dr. Kreger.
The problem with both Parkinson’s and essential tremor is they slowly worsen over time. We don’t have a treatment for that. We can’t slow it down. We can’t stop it. All we can do is treat the symptoms, whether it’s medication, exercise or deep brain stimulation.”
Chief, Neuroscience Institute and Neurosurgery

Christopher DeMassi, MD, FACS, (far left) and Tarek Zakaria, MD, (far right) use the ROSA non-invasive diagnostic tool during an epilepsy procedure.
Epilepsy Program Continues to Innovate
Memorial Neuroscience Institute’s Comprehensive Epilepsy Program has seen tremendous gains in several key areas over the past year.
First, the National Association of Epilepsy Centers recertified the program’s Level 4 ranking — a designation for programs that offer the highest level of comprehensive and specialized care.
And to further the program’s growth, the epilepsy program brought on board fellowship-trained epileptologist Donald Barr, MD. Dr. Barr will expand the program to Memorial Hospital West and into the West Broward region. Dr. Barr has special interest in brain modulation and brain responsiveness stimulation as a treatment option for patients with intractable epilepsy.
“We have a multidisciplinary team that now consists of adult epileptologists, pediatric epileptologists, neuropsychologists, neuroradiologists, neurosurgeons and psychologists," said Tarek Zakaria, MD, Medical Director, Comprehensive Epilepsy Program and Adult Neurology. "We meet every month to discuss individual patients and their treatment options. This is very important communication to be sure that we are providing the best care to our patients.”
Innovative Technology
Over the past year, the program also has implemented some of the most advanced technology-based protocols to diagnose and treat patients with epilepsy. One example is ROSA, or Robotized Surgical Assistant, a non-invasive diagnostic tool that allows neurosurgeons to localize the seizure onset without opening the skull and exposing the brain.
This specific procedure opens the door for multiple treatment options, including surgery to remove the onset zone or implementing a NeuroPace. Memorial’s epilepsy program was the first center in South Florida to use this small, battery-powered “pacemaker of the brain” that is implanted in the skull to record electrical activity and send electrical impulses to the brain to prevent seizures.
Patients tend to tolerate the procedure very well and go home the next day.”
Medical Director, Comprehensive Epilepsy Program and Adult Neurology
Dedicated Stroke Clinic Helps Patients Avoid Additional Strokes
Memorial Stroke Clinic opened in 2020 to provide follow-up care and guidance for patients and help reduce their chances of suffering another stroke.
The dedicated stroke clinic is part of the Comprehensive Stroke Program at Memorial Neuroscience Institute, where approximately 1,900 patients are treated every year. Combining initial high-quality, acute treatment with a thorough diagnostic workup on potential etiologies, or causes, is key to secondary stroke prevention.
“Our goal is to review the patient’s history for any modifiable stroke risk factors, such as high cholesterol, smoking, diabetes and high blood pressure. We want to make sure that patients are on the right medications to address these risk factors,” said Brijesh Mehta, MD, Medical Director, Comprehensive Stroke Program and Neuro-Interventional Surgery.
He added: “Beyond the medical issues, we also want to make sure that if a patient needs ongoing speech, occupational or physical therapy, they’re receiving care at Memorial Rehabilitation Institute following discharge. We’ve seen that this plays such an important role in getting patients back to their prior neurological function and quality of life.”
The clinic is also an educational platform for physicians to observe and practice the continuity of care that is so important in stroke recovery. Neurology residents work closely with neurologists from the Memorial Neuroscience Institute to learn all aspects of the patient’s experience, from the initial acute treatment to rehab and recovery.

Eric, who suffered a stroke.
Grateful Patient Receives Lifesaving Stroke Treatment at Memorial
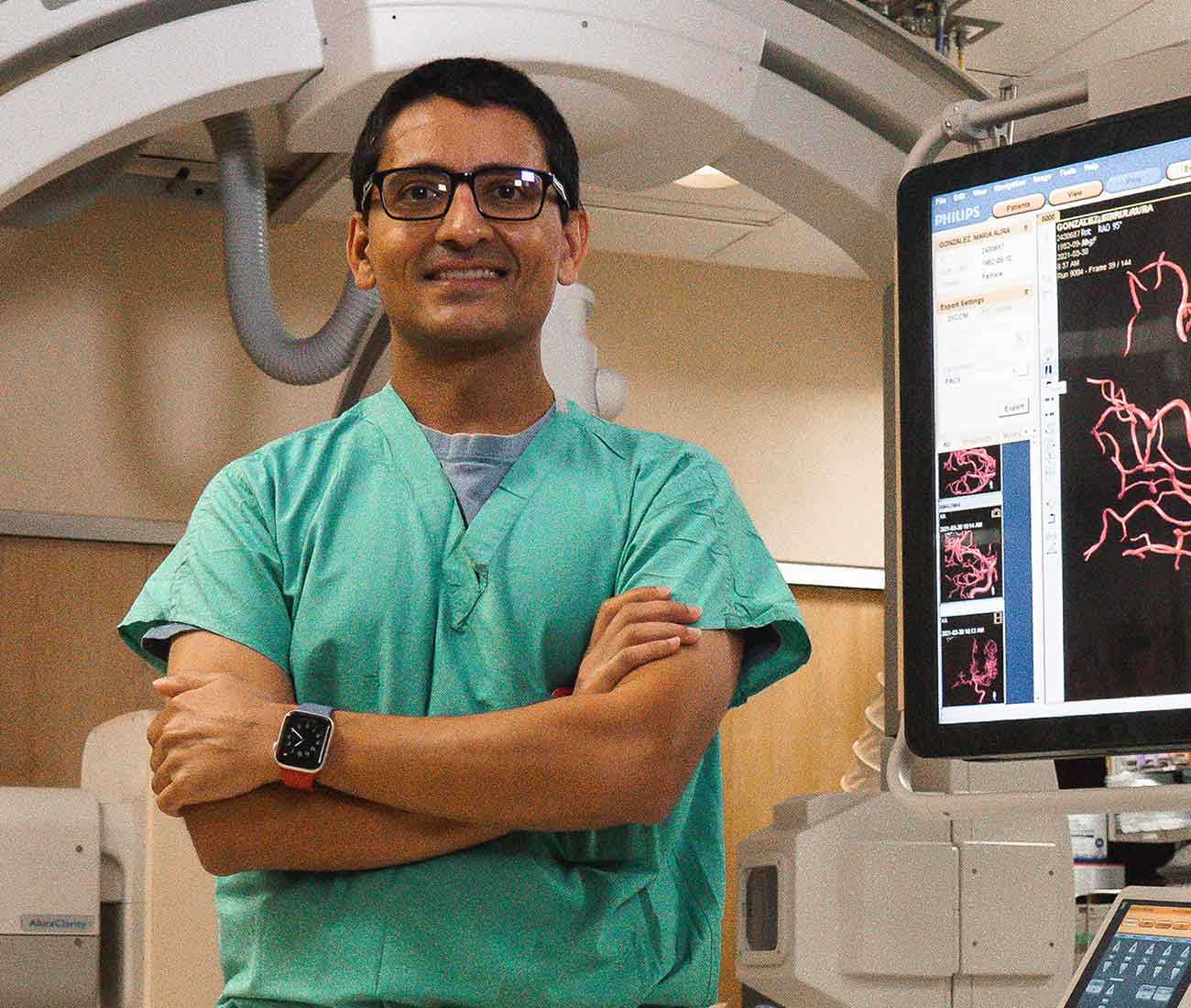
Brijesh Mehta, MD, Medical Director of the Comprehensive Stroke Program and Neuro-Interventional Surgery, diagnosed Eric with “a perfect storm” that led to his stroke.
A CT scan of Eric’s brain and a CT arteriogram revealed that the 29-year-old had a blood clot obstructing flow to the right side of his brain. Diagnostic work-up revealed he had a small hole between the two upper chambers of his heart, as well as a blood clotting disorder. Combined, these conditions threatened the life of the Broward County firefighter and paramedic.
“Eric suffered a large vessel stroke, which is not very common in young patients. In these situations, unfortunately, the clot-busting medication, IV tPA, is not as effective. The blockage of the artery was so extensive that he needed a clot retrieval procedure in the cath lab called mechanical thrombectomy,” said Dr. Mehta.
This procedure, which has been around only for a few years, is now the standard of care because of its effectiveness in opening major blockages of arteries in the brain.
Eric had been working out at the gym that day when he started experiencing paralysis on his left side. First his thumb wouldn’t move. Then he lost function in his left leg. His trainer called 911 when he saw that Eric’s face was drooping, followed by weakness in his arm and leg on one side — classic signs of stroke.
He was rushed from the gym to Memorial Hospital West, where Dr. Mehta and his team quickly diagnosed and treated the young man.
“With Eric’s situation,” said Dr. Mehta, “it was the best of both scenarios: He came in early after the onset of symptoms, and he had good collaterals going to the affected area. It takes so many different parts to deliver timely treatment. Everyone works together to make this a seamless process.”
Today, Eric is regaining his strength and experiencing no functional or neurological deficits. He’s back at the gym, nailing the rope climb and pumping iron.
“Dr. Mehta, along with the other team members who were involved at Memorial, saved my life. I am in a much better position than I was before,” said Eric.
MEMORIAL TRANSPLANT INSTITUTE

Making Miracles During a Pandemic
While some medical centers postponed transplants indefinitely during the pandemic, Memorial resumed performing procedures and saving lives through organ transplantation.
During fiscal year 2021, they made miracles happen for 64 people through heart and kidney transplants. This included performing two pediatric heart transplants within 24 hours — twice — and performing four kidney transplants within 48 hours.
“I’m very proud of our team for believing and doing the right thing for our patients, each other and the community,” said Juan Arenas, MD, Chief of Memorial Transplant Institute. “They have been flexible and also extremely compliant with additional safety precautions to protect themselves and our patients. Everyone continues to be resilient.”
One of the challenges during the pandemic, Dr. Arenas said, was ensuring everyone involved — from staff to patients and their families — were willing to comply with additional safety precautions that were critical for transplant patients because of their weakened immune systems.
Despite the risks, surgeons knew many transplants were urgently needed.
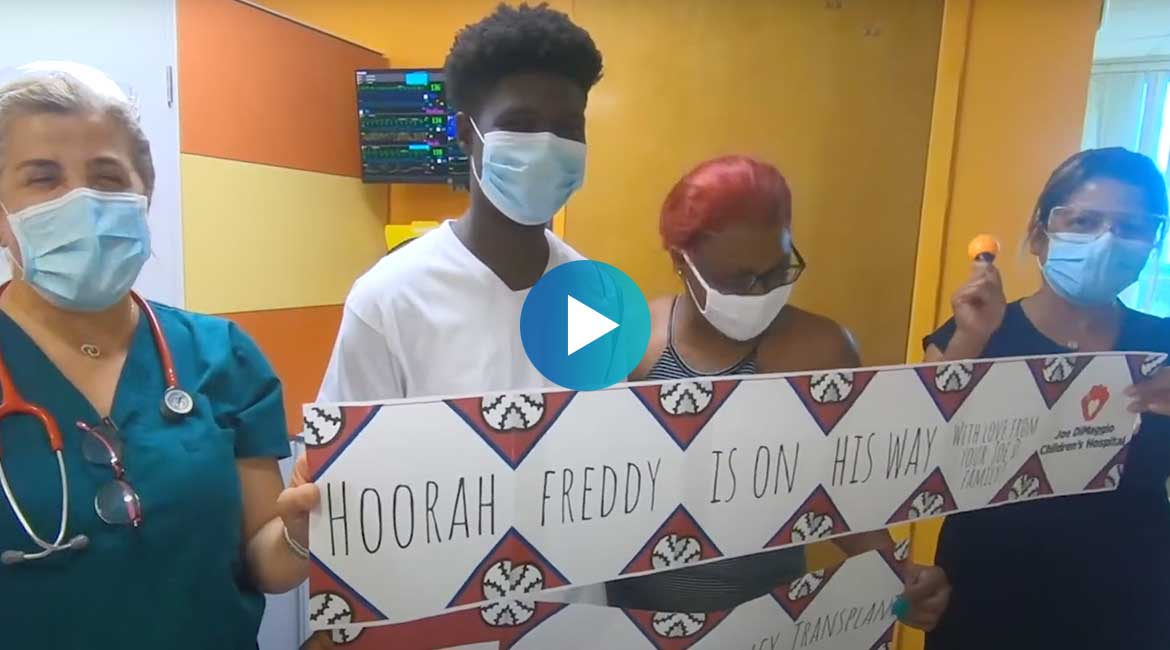
100th Kidney Transplant Gives Teen a New Lease on Life
Seventeen-year-old Freddy was shocked when he got the call from his doctors at Memorial Transplant Institute, alerting him that they found him a new kidney.
“It was like, dang, I really got a kidney,” he said, recalling the moment with a smile.
Freddy’s surgery marked a significant milestone for the Transplant Institute as well — its 100th kidney transplant.
Freddy suffered from kidney failure and said he couldn't have made it through the entire ordeal without the support of his care team at Joe DiMaggio Children’s Hospital.
“My doctors and their staff, they were another support system that I needed,” he said.
His family is grateful for everyone involved, added his mother, Beyonka.
“They made us feel at home,” she said. “We appreciate everything — the support team, doctors, the family that even gave up the kidney.”
Now, instead of worrying about his health, he’s dreaming about his future, which his mom hopes will include playing football again.
“We work as a big team to provide the great care that we offer here,” said Reem Raafat Qbeiwi, MD, medical director of pediatric kidney transplant at Joe DiMaggio Children’s Hospital. “It’s not just a gift to the children, but it’s a gift for the family.”
Juan Arenas, MD, chief of the Memorial Transplant Institute, agreed. “Every time we give someone a new organ, we give them a new lease on life,” he said.
A Second Opinion Leads to a Second Chance at Life
Two years after giving birth to her baby, Nancy knew something wasn’t right. She was always extremely tired and too fatigued to take her baby to the park or go swimming. Then she began to feel chest pains.
After several trips to the hospital and struggling to get answers, her aunt recommended that she go to Memorial Cardiac and Vascular Institute for a second opinion. Her Memorial doctors diagnosed heart failure.
“She was young when she was diagnosed, unfortunately, and in spite of treatment she did not progress the best way and ended up in the transplant list,” said her doctor, Iani Patsias, MD, a cardiologist on the Advanced Heart Failure and Transplantation team.
Nancy’s husband, Javier, said the Memorial team was there for them every step of the way.
“They explained to us the whole process, what was her condition, what was the tests that she needed to undergo,” he said. “They just guide us, step-by-step.”
Fortunately, Nancy did not have to wait long for a heart, and the transplant surgery and recovery went smoothly.
“She’s very happy and doing very well, and we expect that to continue,” Dr. Patsias said.
Two years post-transplant, Nancy and her husband said everything has changed.
“Now, we are able to go out. She’s able to run. She’s doing swimming. We’re doing biking. We’re going to the park. She’s able to do the stairs,” he said. “She’s able to function now.”
Nancy and her husband said they have the nurses, specialists, surgeons and everyone at Memorial to thank.
“We are just so blessed,” Javier said, “and we are just grateful with the whole Memorial team.”
Terique and Family Enjoy Their ‘Rainbow Moment’ After Successful Transplant
Terique was a high school football player -- attending two practices a day – when he began to experience chest pains and shortness of breath.
“He would go home and fall asleep fully dressed in his uniform, with the exception of his helmet,” said his mother, Carrie.
The family turned to specialists at Joe DiMaggio Children’s Hospital for help.
“Terique first came to us pretty sick,” said Svetlana Shugh, MD, pediatric cardiologist. “He had something called myocarditis, where there is infection and inflammation of the heart, and as a result, his heart wasn’t working properly.”
Terique had several recurrent episodes that landed him in the hospital. In one scary instance, his heart stopped beating. The heart muscle was seriously damaged, and he was put on the transplant list in hopes of finding him a new heart.
“I was scared,” Terique said. “I wanted to live life, but I can’t because I have a bad heart.”
Terique’s parents still remember the day they received the call that a heart had been found — Oct. 3, just days before his mother’s birthday.
“He kind of just flew through the transplantation and was able to be discharged pretty quickly,” said Laura D’Addese, MD, pediatric cardiologist, and heart failure and transplant specialist. “He’s doing great.”
The transplant was a turning point, Terique said. “Today I feel better than ever. It’s a blessing.”
His father agreed. “After the storm comes the sun, the sunlight and rainbow,” he said. “We’re in our rainbow moment right now.”
PEDIATRIC SERVICES

Gerson, who had a heart transplant, and Lana Shugh, MD, Pediatric Cardiologist
10 Years of Pediatric Heart Transplants

In December, the Joe DiMaggio Children’s Hospital Pediatric Heart Transplant Program celebrated 10 years of providing new hearts and second chances to children and teens suffering from heart failure.
“It has been a really joyous ride,” said Maryanne Chrisant, MD, medical director of Heart Transplant, Heart Failure and Cardiomyopathy at Joe DiMaggio Children’s Hospital Heart Institute. Dr. Chrisant was brought on board in 2010 to develop and grow the program.
“Even last year with COVID, we left our doors open, and we were able to do transplants for a lot of children,” she said.
Frank Scholl, MD, Chief, Joe DiMaggio Children's Hospital Heart Institute, said that transplant patients may have been at a slightly higher risk for COVID-19, but they were at a much higher risk of dying due to their heart failure. So the transplant team worked hard to overcome the challenges and kept transplants going.
“It comes down to leadership and discipline with the whole team to make organization out of chaos,” Dr. Scholl said. “We kept the patients’ best interests at heart, and we figured out a way to make it work."
The pediatric heart transplant team has grown as cardiac experts were recruited from around the country. The team’s expertise spans multiple disciplines, including congenital heart care, cardiomyopathy, advanced heart failure, critical care and mechanical circulatory support.
“This team cares about the patients, the families and each other in a very special way,” said Dr. Scholl, who performed the first pediatric heart transplant in Broward County at the hospital.
Data from the program shows that patients do exceptionally well, even beyond the critical three-year post-transplant survival rate and despite the fact that they often have complex cases.
“Our outcomes are as good as or better than any other program in the country,” Dr. Scholl said.
Dr. Chrisant said the support of Memorial’s leadership and the entire team has a huge influence.
“So much of what contributes to our success is the care and support our patients and families get before, during and after their transplant from everyone here at Memorial,” she said.
2021 Heart Transplants

Baby Kayden received complex care during the COVID-19 pandemic.
Maintaining Focus and Flexibility
When the COVID-19 pandemic hit, elective and non-emergency surgeries were suspended at Joe DiMaggio Children’s Hospital. The number of patients quickly diminished. And many team members were redeployed to the front lines, caring for adult patients in other Memorial hospitals, emergency departments and the COVID-19 drive-through testing site in C.B. Smith Park.
Visitors and family members had to be restricted like never before — a stark and distressing change for a children’s hospital that has always involved families and caregivers in all aspects of care and operations.
Instead of focusing on the obstacles at hand, team members put their attention and energy into supporting their colleagues serving adult patients, preparing for how COVID-19 might affect children and teens, and perfecting the children’s hospital’s quality and safety protocols to enhance care.
“One of the most remarkable things to me was how far we have been able to advance our quality and safety programs during the pandemic,” said Ronald Ford, MD, MBA, Chief Medical Officer. “We have always had this culture of safety, but we made tremendous advances in expanding our programs during the pandemic. There was such a high level of engagement from our physicians and staff.”
Joe DiMaggio Children’s Hospital is part of the Solutions for Patient Safety (SPS), a group of more than 150 children’s hospitals working together in an all-teach, all-learn format to improve hospital processes and outcomes. While quality and safety data at Joe DiMaggio Children’s Hospital have always been impressive, the Heroes for Zero initiative is always striving for a zero-harm environment.
At the same time, teams also prepared for how COVID-19 might affect children and adolescents. The focus was on multisystem inflammatory syndrome, also known as MIS-C, which became apparent in some children with COVID-19.
“Even before we saw the first case, we set up a multidisciplinary team that had connected with other experts from around the world — including Italy and the U.K. — to learn from their experience. We created a plan for how to best care for and treat these patients,” Dr. Ford said. “So when we had our first patients present with this, we were ready.”
That multidisciplinary team included specialists from cardiology, infectious disease, critical care, immunology and others.
“Throughout it all, everyone, despite everything that was coming at them every day, was so resilient and nimble. I am so astounded by their resiliency,” Dr. Ford said.
COVID-19 Effect on Children
To date, Joe DiMaggio Children’s Hospital has cared for 74 children with COVID-19 who developed MIS-C, or multisystem inflammatory syndrome. The multidisciplinary care team also is participating in a national study with other medical centers. The study will follow these children over the next few years to examine possible long-term effects of the virus and to improve treatment plans.
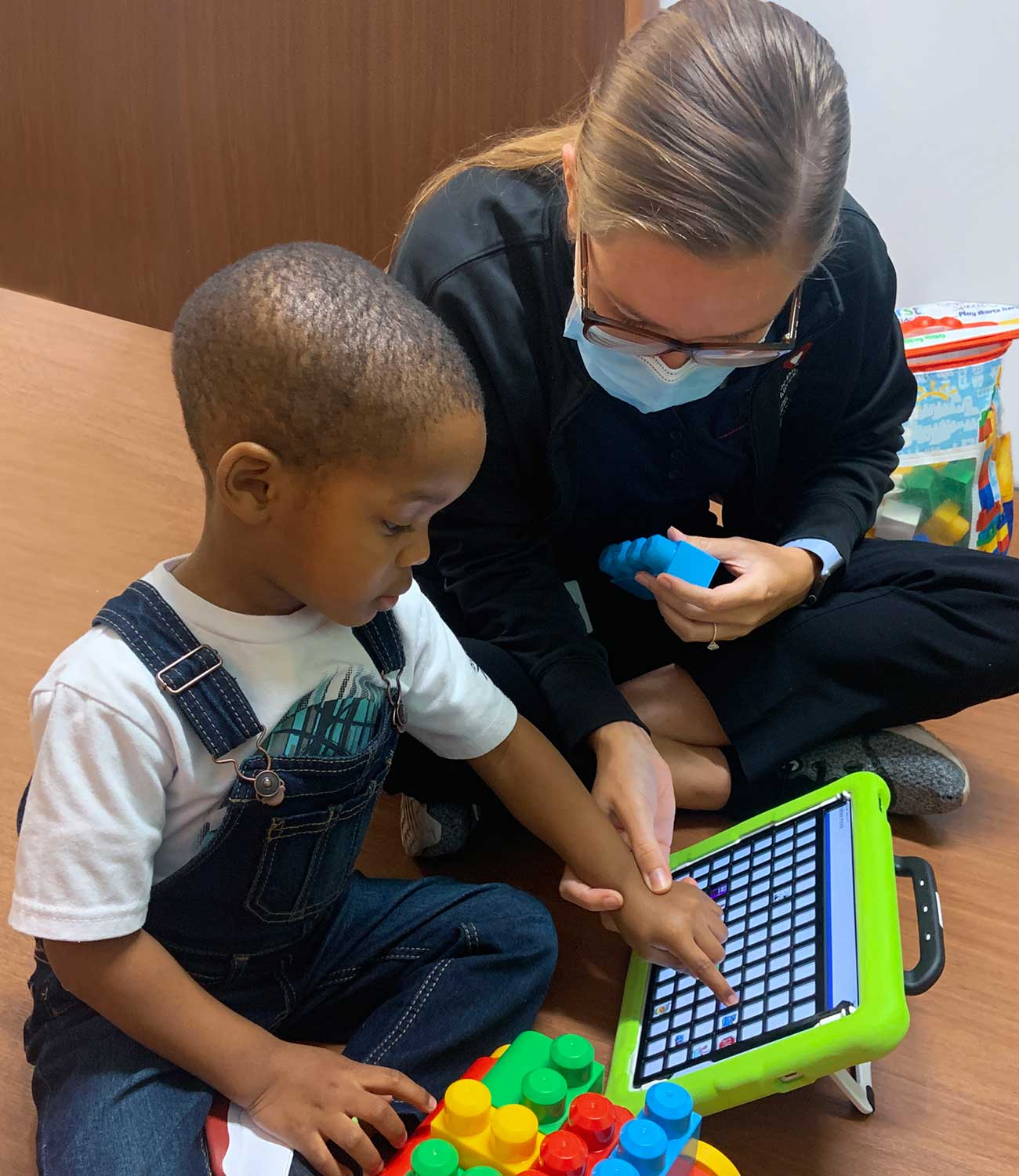
A rehabilitation session at Joe DiMaggio Children's Health Specialty Center in Wellington.
Serving Families Close to Home
Joe DiMaggio Children’s Health Specialty Center in Wellington continues to expand its services and programs to meet the needs of children and adolescents in Palm Beach County.
The 33,000-square-foot facility is a specialty clinic where patients can access doctors with expertise in a broad range of specialties. Within recent months, the center added a Cystic Fibrosis Clinic, and services include therapy/ rehabilitation, imaging including MRI and ultrasound, and an outpatient surgical center.
“Our overall goal for this location, and one of the reasons we opened it, was to keep the care closer to home for as many kids as possible,” said Dawn Quaranta, Vice President of Regional Operations for Joe DiMaggio Children’s Hospital.
The center also helps to coordinate care for children with complex and chronic conditions, allowing them to see multiple specialists at the center.
“We’re listening to the community — families, local pediatricians and providers — to find out what services are needed and what needs aren’t being met, and work to bring those services to our families,” Quaranta said. “We also coordinate and partner with local pediatricians, specialists and providers to connect patients to other services that we may not have at our Wellington facility. In the end, our goal is to work together to care for our community.”


Luis, who had a cleft lip
20 Years of Caring for Children with Facial Differences
Since opening its doors in 2001, Joe DiMaggio Children’s Hospital Cleft and Craniofacial Center has been improving the lives of children with facial differences.
The center has become a leading craniofacial center in the nation. The team cares for children with cleft lip, cleft palate, craniosynostosis and other conditions involving the face and head.
Since the start of the coronavirus pandemic, the team reorganized the clinic without significant disruption to continue providing care through telehealth and inperson visits. It continues to provide comprehensive, multi-specialty in-person care to about 50% of its patients each week.
The center also expanded services to Joe DiMaggio Children’s Health Specialty Center in Wellington, where it runs a monthly clinic that allows families living in Palm Beach and surrounding areas to access the same great care closer to their home.
“We provide comprehensive care not only to our patients but to the entire family who has to deal with a patient’s special needs,” said Roman Yusupov, MD, Medical Director and pediatric genetics specialist.

Rendering of the expanded Joe DiMaggio Children's Hospital
Catch the Love Campaign on Its Way to $56M Goal
The nonprofit Joe DiMaggio Children’s Hospital Foundation has established a $56 million capital campaign goal to help support the vertical expansion of Joe DiMaggio Children’s Hospital from four to eight floors. By May 2021, the organization raised more than $35 million through the Catch the Love campaign.
The number 56 is symbolic, as it reflects Joe DiMaggio’s hitting streak across 56 consecutive games in 1941. The Yankees player’s record remains unbroken.
“It was important to us that philanthropy significantly contribute to the estimated $170 million cost of the children’s hospital expansion, since donors have made it clear they are committed to having the space and resources to be the finest pediatric facility in America,” said Andrew Greenfield, MD, board chairman of the Joe DiMaggio Children’s Hospital Foundation.
Construction at the children’s hospital is ongoing, with estimated completion in late 2022. The additional floors will feature 72 new patient rooms, two cardiac hybrid operating rooms, two surgical suites, intensive care and cardiac intensive care units, an intraoperative MRI, play zones, rehabilitation and family support areas.
“This project will ensure that Joe DiMaggio Children’s Hospital remains uniquely qualified to treat the most complex and critical conditions, so that South Florida kids and families won’t have to travel elsewhere to receive quality medical care,” said Brett Rose, campaign chairman. “By making a gift toward our goal, donors are ensuring the future of a critically important resource and personally making a difference in our community.”
Joe DiMaggio Children’s Hospital is one of the nation’s leading pediatric hospitals and is ranked by U.S. News and World Report. The children's hospital offers a comprehensive scope of healthcare services and programs in a caring, compassionate setting designed specifically for children.
“They do a remarkable job of making the hospital not feel like a hospital,” said Jeff Conine, a former major league ballplayer who knew Joe DiMaggio and has been a philanthropic supporter of the children’s hospital for more than 25 years. “They treat you like family, and Catch the Love embodies the belief that together we can create something even more special.”
Will you help us meet the healthcare needs of South Florida’s children and their families? Donate at JDCH.com/Give.
Joe DiMaggio Children's Hospital Expansion
Construction is underway, with estimated completion in late 2022.

Orthopedic Center Expands Reach and Services

Joe DiMaggio Children’s Hospital Orthopedic Center continues to enhance and expand its services, resulting in the hospital being ranked the top children’s hospital in Florida for orthopedics by U.S. News & World Report for the third year in a row.
The center has the largest group of fellowship-trained pediatric orthopedic specialists in South Florida. The team has grown from one physician to 10 over the past three decades and has about 60 employees with six locations, stretching from southern Broward to Palm Beach counties.
“All of the members of our team are trained at the leading children’s hospitals in the nation, and our department is now equal to any of them,” said Michael Jofe, MD, Surgeon-In-Chief at Joe DiMaggio Children’s Hospital and Chief of the Department of Pediatric Orthopedics. “We are now one of the busiest and most comprehensive programs in the country.”
“At Joe DiMaggio Children’s Hospital, patients and families can receive world-class care in one location,” he said. “Memorial and Joe DiMaggio have the best medical specialists and staff to cover all patient needs and enable us to collaborate and deliver comprehensive care across all specialties.”
Orthopedic Program Growth
The Orthopedic Center is home to several specialized programs including spinal deformity, sports medicine, hip preservation, limb lengthening, performing arts and dance medicine, and a concussion clinic.
“With every new physician who joins our practice, we are able to expand our services and specialties,” said Melissa Vale, Director of the Orthopedic Center.

The two newest members of the orthopedic surgery team — Michael Aversano, MD, and Andrew S. Gupta, MD — have created a new Hand and Upper Extremity Program to provide specialized care for children and adolescents with traumatic and congenital conditions. See related story.
The Center for Hip Preservation is a nationally recognized resource for patients from infancy to young adulthood for the care and treatment of congenital and acquired hip conditions, hip dysplasia and femoroacetabular impingement. It is one of the few comprehensive programs in the country, due to the specialized training and expertise required to perform the complex procedures and the resources necessary for pre- and post-operative care.
The concussion program also continues to expand as the community’s needs grow. Specialists now consistently see several patients every day with sports-related concussion injuries.
“Having so many subspecialists within the orthopedic department and at Joe DiMaggio Children’s Hospital elevates the experience for patients and providers alike,” Dr. Gupta said.
COVID-19 Response
The orthopedic team also had to overcome many challenges due to the COVID-19 pandemic throughout the year. The cancellation of elective and nonessential surgeries affected many programs.
“For the past year, inpatient and elective surgeries have been severely limited,” said Dr. Eric Eisner, a pediatric orthopedic surgeon who specializes in hip preservation. “We’ve utilized the excellent physical therapists in the [U18] Rehabilitation Center, in addition to expanding our telehealth services, to help with the management of symptoms while waiting to do surgery on patients.”
Leaders from the Orthopedic Center also provided pandemic guidance for local schools. They served with other community healthcare organizations on the Broward County Public Schools Sports Medicine and Student Wellness Advisory Committee and provided guidance on COVID-19 mitigation protocols throughout the pandemic, helping students return safely to sports activities.
“During the pandemic, we helped the Broward County District Schools develop screening processes, manage positive cases and exposures, gave guidance on how to safely get sports off the ground and shared best practices provided by national medical organizations,” Dr. Fazekas said. “We were able to get athletes back to doing what they love safely and even participate in a tri-county championship.”
The practice also embraced telehealth and continued to see patients virtually, if possible, based on the injury or concern.

I am proud of the way we have been able to provide world-class care while being safe for our patients, staff and the community throughout the COVID-19 pandemic.”

Orthopedic and sports medicine care includes specialized services for performance arts and dance.
[U18] Sports Medicine Program Expansion

The [U18] Sports Medicine Program continues to flourish. It expanded its school sports outreach program, making it one of the largest school-based athletic training programs in the country.
Twelve schools joined the program, bringing the total number of public high schools covered to 41, spanning Broward and Palm Beach counties.
“Our team has a vision of being able to provide best-practice services to athletes even beyond the scope of our own program,” said Matthew Fazekas, MD, FAAP, CAQSM, Medical Director of the Pediatric Sports Medicine Program. “Despite COVID, despite school districts modifying athletics and school itself, we’ve still grown to provide Certified Athletic Trainers for about half of Palm Beach County. This is not something you see happening in a lot of other communities.”
The program also offers student athletes guidance on injury prevention, injury assessment and evaluation, connections to pediatric orthopedic specialists and rehab services at Joe DiMaggio Children’s Hospital and return to play evaluations at their schools.
Advocating for Athletes in Florida and Beyond
Members of the orthopedic and sports medicine team are advocating and providing care for athletes on a state, national and international level. In addition to working with Broward County schools, Dr. Fazekas serves as a board member for the Florida Alliance for Sports Medicine and as a consulting physician for USA Figure Skating.
Michael Dressing, MD, is a consulting physician for USA Soccer and is an affiliate team physician for the Washington Nationals major league baseball team.
This past year, Jeremy Frank, MD, has continued to travel internationally with the United States National Wrestling Team, serving as a team physician. He’s been working with the team for more than 14 years, and this year traveled to both France for the French Grand Prix and Norway for the World Wrestling Championships.
“My specialty is taking care of pediatric, adolescent and young adult athletes who get injured and either surgically or non-surgically help them get back to full function," Dr. Frank said. “It’s an honor to take care of people who represent the United States and to represent Memorial and Joe DiMaggio Children’s Hospital while doing so.” Any family with a child with orthopedic needs can feel secure in knowing that they will get worldclass care at the Joe DiMaggio Children’s Hospital Orthopedic Center.

Matthew, who had shoulder surgery.
Hand and Upper Extremity Program Grows

Joe DiMaggio Children’s Hospital Hand and Upper Extremity Program continued to expand in its first year, growing its staff of highly specialized experts who care for children, adolescents and teens.
The program, which started in 2020, is part of the hospital’s Orthopedic Center — the largest group of fellowship-trained pediatric orthopedic surgeons in South Florida.
The Hand and Upper Extremity team — led by pediatric orthopedic surgeons Michael Aversano, MD, and Andrew S. Gupta, MD — cares for children with sports-related and traumatic injuries, as well as those with neurological and congenital conditions that affect the hand, wrist, forearm, elbow and shoulder.
Drs. Aversano and Gupta have both completed several specialized fellowship training programs to become experts in the care of children and adolescents with hand and upper extremity needs.
“I think that an essential part of the growth of the program and a big part of its success comes from the support of the entire Joe DiMaggio Children’s Hospital community. We’re growing a very specialized team with an emphasis on providing a complete continuity of care experience for our patients,” Dr. Aversano said.
This year, the team welcomed a pediatric interventional radiologist for upper extremity diagnostic and procedural studies.
“We have our support staff, physicians, radiologists, occupational and physical therapists all in one place,” he said. “This environment not only results in better outcomes, but also helps build a better relationship with our patients and families.”
An Evolving Field
The field of pediatric hand and upper extremity surgery is constantly evolving and continues to expand as technology and innovation unite. The children’s hospital team constantly seeks to enhance methods of treatment through evidence-based practice and connect with physicians across the globe to learn new and exciting treatments for hand and upper extremity conditions.
Children and adults have different orthopedic needs that should be considered during care and treatment.
“Kids are still growing, and our treatment must take into account what will happen as they develop,” Dr. Aversano said.
He added: “Medicine is changing and evolving. Everything is becoming more and more specialized, and treatments are becoming more complex as we learn new and exciting things. It is our goal at Joe DiMaggio Children’s Hospital to be at the forefront of high-quality and life-changing care both locally in South Florida and nationally.”

Children’s Hospital Receives Highest Surgical Verification
Joe DiMaggio Children’s Hospital received Level I Children’s Surgery Verification from the American College of Surgeons Children’s Surgery Verification Program. The hospital is one of only two in the state with Level I verification and joins an elite list of only 33 hospitals nationwide with this honor.
“Achieving Level I speaks to the caliber of the surgical team at Joe DiMaggio Children’s Hospital and attests to our capability for meeting the most complex surgical needs of our pediatric community,” said Jill Whitehouse, MD, Vice-Chief of Pediatric General Surgery. “It also demonstrates our team’s passion for excellence and our dedication to safety and quality that extends to every patient we touch.”
The verification is given to centers that show a commitment to quality care, have highly trained staff, participate in cutting-edge research and have surgeon leaders who review outcomes throughout the year.
Food Pantry Opens to Help Nourish Hospital Patients and Families
Joe DiMaggio Children’s Hospital is doing its part to stamp out hunger in South Florida. In February 2021, the hospital opened a food pantry for patients and their families to provide healthy, nutritious foods they can take home and that will help in their healing and recovery. Created in partnership with Lions Club International and Feeding South Florida, the Food Pantry is expected to benefit about 750 families in 2021.

MEMORIAL FAMILY BIRTHPLACE

NICU nurse Jodi Tidwell, RN, and respiratory therapist Rosa Gallego with baby Emma Elizabeth
OB and NICU Collaborate on Care Delivery
Collaboration between pediatric specialists at Joe DiMaggio Children’s Hospital and obstetrical teams at Memorial Healthcare System enables the delivery of highly personalized care to mothers and their babies born with complex medical conditions.
In December 2020, the teams collaborated to successfully perform an ex-utero intrapartum treatment procedure — also called an EXIT procedure — in which doctors provided care to a newborn during birth via cesarean section.
“The entire team invested months of preparation to get it right,” said Holly Neville, MD, Chief of Pediatric General Surgery and Associate Program Director of the Surgical Residency Program.
Coordinated Care for Complex Pregnancies
When a woman has a pregnancy that is considered high risk or other maternal and/or fetal complications arise, they are referred to Memorial’s Maternal-Fetal Medicine program run by Laurie Scott, MD.
The program coordinates care between Memorial OB specialists and pediatric specialists at Joe DiMaggio Children's Hospital — including those from the Wasie Neonatal Intensive Care Unit, which provides Level ll and Level lll neonatal intensive care services for about 850 babies a year. Together, they provide seamless, expert care for both mother and baby throughout the pregnancy, birth and beyond.
Pediatric specialists also meet with the mom-to-be and family prior to the delivery to answer questions about the treatment and care that may be required for their child once the baby is born.
"We meet monthly with perinatology, nurse navigators, neonatology, pediatric cardiology and pediatric surgery to create and refine care plans,” said Lester Mc Intyre, MD, Chief of Neonatology. “The key is anticipation, so you know what you’re dealing with and you have all of the necessary resources available.”
Nurse navigators arrange care throughout the process and alert all doctors, nurses and specialists involved with the patient as the pregnancy progresses and when a mom is set to deliver.
“Everyone knows the plan of care; all of the subspecialists and providers are kept in the loop. We all have the plan and know what will happen the second the baby is born,” said Janessa Alonso, MSN, MHA, RNC-NIC, Director of Nursing in the NICU.
If unknown complications arise during a delivery, the NICU team is notified immediately and on hand to provide the emergency care needed.
“There is an established relationship between the OB and NICU teams,” said Barbara Glassman, MSN, Clinical Project Manager in the NICU. “On the nursing side, we are in constant communication throughout our shifts, so when something arises, collaboration is natural.”
Once a baby is delivered, mom and baby both have access to the specialty care they need in one place.
“Since the care plans are refined each month, there is a seamless handover that happens at the time of delivery,” Dr. Mc Intyre said.
Family Birthplace Deliveries
EXIT Procedure
The collaborative processes between pediatric specialists at Joe DiMaggio Children’s Hospital and obstetrical teams at Memorial Healthcare System were critical when they came together to perform the first EXIT procedure at Memorial. The procedure was performed to successfully deliver a baby with a mass on the tongue that would interfere with the baby’s ability to breathe. Pediatric ENT and head and neck surgeon Sweeti Shah, DO, was able to intubate the baby during the C-section, while the baby was still attached to mom via the placenta for support.
Since the procedure was a first at Memorial, the team prepared for months, doing research, planning and performing run-throughs.
“Everyone brought their knowledge and practical experience together for the benefit of these patients,” said Dr. Neville.
After the C-section, the baby was brought to the NICU and is now being followed by Dr. Shah.
Dr. Neville said this is a perfect example of the collaborative care delivered at Memorial. “Everyone went above and beyond for that baby.”

Baby Serenity and her mom
MEMORIAL SURGICAL SERVICES

Ryan, who had weight-loss surgery as a teen, and Brett Cohen, MD
Weight-Loss Surgery Program for Teens
The new Joe DiMaggio Children’s Hospital Adolescent Weight-Loss Surgery program is helping teens and young adults lose weight and gain confidence with specialized programs tailored to meet their unique needs.
While surgeons at Memorial have performed weightloss procedures on adolescents in the past, they realized that teens have different needs from adults and had nowhere to turn for specialized services and support.
“Young adults are in a different place in their life and have different needs than adults,” said Brett Cohen, MD, Chief of Adult General Surgery and Bariatric Surgery at Memorial. “And there aren’t many programs out there tailored to meet their emotional, psychological and physical needs, as well as the support that can help them achieve their long-term health and weight-loss goals.”
Since the program’s inception in 2020, surgeons have helped more than 30 young adults lose weight via sleeve gastrectomy, a type of bariatric surgery in which part of the stomach is removed, limiting food intake. Others have utilized our medical weight-loss programs for patients who do not qualify for or want to undergo surgery.
The program has been successful thanks to the collaborative team approach by the surgical teams and pediatric specialists, including Lital Reitblat, MD, Pediatric Endocrinologist, who works with teens and young adults before and after surgery.
"I promise them that I'm going to be with them throughout this journey," Dr. Reitblat said. "We take into consideration the multiple things that adolescents need. We provide that sort of wraparound care."
All patients must go through a four-to-six-month program before undergoing surgery. They work with a mental health specialist and nutritionist, both of whom are experienced in working with young adults.
“The program is about much more than an operation. It’s about making changes, and the surgery makes these changes easier to be successful with,” Dr. Cohen said.
It’s a dramatic change for these young adults. It’s changing their overall view of themselves and their approach to life in general. They are much happier in their own shoes. You feel like you’ve helped them make a change that will affect them for many years to come.”
Chief, Adult General Surgery and Bariatric Surgery
Weight-Loss Surgery Helps Teen Gain Health and Confidence
Ryan remembers being 308 pounds with diabetes, high triglycerides and high cholesterol, struggling with his health and confidence but unable to shed the weight.
“I hated photos. I didn’t want anything to do with a picture,” he said. “I would hide behind people. I would put things in front of me.”
The weight-loss process felt like an emotional roller coaster, he said. He would lose weight only to gain it back again. He tried medications and programs, but nothing worked.
“Being a Type 2 diabetic, I was trying to lose weight, but my body wouldn’t let me,” he said.
He turned to the surgeons at Joe DiMaggio Children’s Hospital’s Adolescent Weight-Loss Surgery Program for help.
“He came to us as one of our first adolescents,” siad Brett Cohen, MD, Chief of Bariatric Surgery at Memorial Healthcare System. “Ryan always had a smile on his face. He’s a really good kid, and he struggled. He already had started developing pretty significant issues associated with the weight.”
After weight-loss surgery Ryan made the necessary changes to drop 100 pounds, including routine exercise.
“Losing all that weight in the first year was such a confidence booster,” Ryan said. “I look in the mirror, and I look great. I don’t have health problems anymore. All of the ramifications for being overweight were just so grave, and all of it is dissipated. It’s gone.”
Now, Dr. Cohen said Ryan seems like a different person.
“The power of the procedure is just amazing because it has changed my life in so many ways,” Ryan said, “and I feel so free and happy.”
Memorial Welcomes Female Surgeons to General Surgery Team
Two female surgeons have joined Memorial Healthcare System’s general surgery team. Mia Shapiro, MD, joined Memorial in 2019 and Kristina C. Khazeni, MD, in 2020.
While the number of female medical students and doctors continues to rise, women have remained underrepresented in many surgical fields. That is changing.
“The trends in representation in the field of surgery have changed dramatically across the United States,” said Dr. Shapiro. “I went to school in New York, and in my graduating general surgical residency class, I was one of eight female chiefs in an all-female class. While the hospital surgical department was predominantly male, there were women represented in each specialty and plenty of female mentorship.”
“I think that as a whole, the surgical fields have become more family-friendly, which has led to an increase in the number of female surgeons,” said Dr. Khazeni.
As general surgeons, Drs. Khazeni and Shapiro join the Memorial team in caring for patients with a wide variety of conditions and ailments.
Dr. Khazeni specializes in intra-abdominal pathologies and hernias, and cancer.
Dr. Shapiro treats soft tissue conditions and performs hernia, gastrointestinal and weight-loss procedures.
“I am lucky to be in a place that takes a collaborative approach to patient care. We strive to do things with the most minimally invasive approach possible so that patients can recover quicker," Dr. Khazeni said.
Now both are looking forward to working with patients, medical students and the community.
“We are looking forward to continuing to grow Memorial’s general surgery practices in South Florida. We will also be opening up a bariatric surgery office in the Midtown Miami area, and I am looking forward to increasing access to what I believe is life-altering surgery,” Dr. Shapiro said.
A Leader for Hernia Surgery
Memorial Healthcare System Hernia Program is working toward becoming a Center of Excellence and continues to offer specialized and personalized care for patients.
The center is home to surgeons with expertise in hernia treatment using standardized procedures and offering a unified approach to care. While the COVID-19 pandemic slowed the certification process, the team hopes to become a Center of Excellence by the end of 2021.
The initial program was a pilot out of Memorial Hospital Pembroke with four surgeons but now includes surgeons at other Memorial hospitals as well.
“This program has enhanced our ability to work together using the latest, evidence-based protocols, helped us improve services as we track our results and provided patients with education and support as they heal,” said Joe Stuczynski, CEO of Memorial Hospital Pembroke.
The center will enable patients to come to one place and find an experienced surgeon who specializes in their specific type of hernia, which is important as hernia procedures become more complex.
“Hernia treatment has evolved immensely, from the tools available to the techniques that we use,” said Jeremy Gallego Eckstein, MD, Medical Director of the Hernia Program and Associate Medical Director of Bariatric Surgery.
The Hernia Program will also be providing a unique, minimally invasive procedure pioneered by Dr. Eckstein at Memorial Hospital Pembroke called Rectus Abdominis Minimization (RAM) that fixes hernias and stretched stomachs in women after pregnancy.
“We don’t box ourselves into one particular technique or technology,” Dr. Eckstein said. “We use everything that is available so that we can create a customized treatment plan for each patient.”
MEMORIAL REHABILITATION INSTITUTE

Memorial Rehabilitation Institute found digital technology and virtual connections to be invaluable during the pandemic.
Embracing Virtual Solutions to Serve Patients
Digital technology and virtual connections proved especially useful to the team at Memorial Rehabilitation Institute during the pandemic. These tools allowed physicians, therapists and nurses to connect with patient families in order to provide virtual training to caregivers and to keep the patient safe after discharge.
"Adaptive sports and recreation activities have continued and are being offered virtually,” said Dawn Broksch, Associate Administrator, Memorial Regional Hospital South.
“These online groups help participants feel less isolated while encouraging them to remain active by considering activities like gardening. These are not necessarily group activities, but things people can do at home to stay active.”
Digital tools also aided professional development and knowledge sharing. Rehabilitation Grand Rounds, Multidisciplinary rounds and Memorial Sports Medicine Journal Club and Lecture series were held virtually to allow multiple locations across Memorial Healthcare System and our community to participate in education.
The virtual Memorial Sports Medicine Journal Club and Lecture Series was established as a means for surgeons, physicians and therapists to exchange ideas and knowledge about the latest clinical evidencebased research and practice in orthopaedics and rehabilitation.
The Memorial Graduate Medical Education Physical Medicine and Rehabilitation Residency Program at the institute remained connected as well. In February, participants “attended” the first virtual conference for the Academy of Academic Physiatrists.
“Although the pandemic has changed some workflows, Memorial Rehabilitation Institute is still able to offer quality programs to our community,” said Douglas A. Zaren, FACHE, Administrator and Chief Executive Officer, Memorial Regional Hospital South, Memorial Rehabilitation Institute and Memorial Rehabilitation Institute Post-Acute Care Network.

AlterG® Anti-Gravity Treadmill™
Orthopaedic Surgery and Sports Medicine Center Opens in Fort Lauderdale
Fort Lauderdale and North Broward County hailed the grand opening of Memorial Orthopaedic Surgery and Sports Medicine Center at the Cypress Creek Medical Pavilion. The virtual opening and ribbon-cutting ceremony took place in March 2021 via Facebook Live.
Centrally located near the Fort Lauderdale Executive Airport, the center is the first of its kind in the area to offer joint replacement surgery in an outpatient surgical facility.
The 9,000-square-foot center is unique since patients can receive evaluations, scans, procedures and physical therapy all under one roof. The multidisciplinary team includes board-certified, fellowship-trained surgeons, physicians and therapists who specialize in sports medicine, joint replacement, fracture care, image-guided injections and physical therapy. They use the latest medical advances to realize individualized treatment plans and to produce quality patient outcome, regardless of age or activity level.
Daniel B. Chan, MD, Chief, Orthopaedic Surgery and Sports Medicine at Memorial Healthcare System is the center’s medical director. He works closely with Marvin Smith, MD, Sports Medicine Orthopaedic Surgeon, and Geden Franck, MD, Sports Medicine Primary Care, who are also part of the center’s topnotch medical team.
“Our outpatient anterior hip replacement surgery has been a game changer for patients. Patients are literally walking within 30 minutes of surgery,” said Dr. Chan. “We’re sending total hip and total knee patients home the same day.”
The new Fort Lauderdale facility follows in the footsteps of the Hollywood-based center at Memorial Regional Hospital South. With the opening of the new center, Memorial’s services and care will reach even more residents in South Florida.
“This facility is very special,” said Dr. Smith. “It allows us to branch out and serve even more of our community and really bring that top-flight orthopaedic care and sports medicine that we’ve been providing for many of our South Broward and Miami-Dade County residents.”

Main Facilities
Memorial Regional Hospital South/Memorial Rehabilitation Institute
Joe DiMaggio Children’s HospitalAncillary Facilities
Conine Clubhouse
Memorial Specialty Services – Aventura
Memorial Specialty Services – Midtown Miami
Memorial Center for Behavioral Health – Outpatient
Pediatric and Adult Outpatient Rehabilitation Center – Hollywood
Memorial Home Health Services
Memorial Home Infusion/Memorial Specialty Pharmacy – Miramar
Adult Pulmonology and Sleep Medicine Center – Hollywood
Memorial Infectious Disease – Hollywood
1Memorial Specialty Services – Weston
Pediatric Specialty Center – Weston
Pediatric Specialty Center – West Boca Raton
Pediatric and Adult Specialty Center – East Boca Raton
Pediatric Specialty Center – Coral Springs
Joe DiMaggio Children’s Health Specialty Center – Wellington
Memorial Orthopaedic Surgery & Sports Medicine Center – Fort Lauderdale
Memorial Weight-Loss Surgery
Memorial Pembroke 24/7 Emergency Care Center
Memorial Urgent Care Center – Pembroke Pines
Memorial Urgent Care Center – Hollywood
Memorial Primary Care – Dania Beach
Memorial Primary Care – East Hollywood
Memorial Primary Care – Hallandale Beach
Memorial Primary Care – Hollywood
Memorial Primary Care – Miramar
Memorial Primary Care – Pembroke Pines
Memorial Primary Care – West Miramar
Memorial Primary Care – Monarch Lakes
Memorial Primary Care – Silver Lakes