Setting the Stage
Memorial's Next 70 Years
When Scott Wester arrived at Memorial as President and CEO in July 2022, the top item on his to-do list was listening.
“As I toured our facilities and attended rounding and discovery sessions, I heard pride in the descriptions of patient care that Memorial provides, and commitment from team members who were fully aware of the responsibility and impact expected from their work,” he says. “And everywhere I went, everyone had a great Memorial story.”
Each encounter and learning opportunity pointed to one inescapable fact: Memorial is a valued community leader and essential partner for everyone the organization touches.
“We are a trusted healthcare brand — the 18th most trusted one in the nation, according to Monigle,” Mr. Wester says. “The community has great faith in what we do and the care we provide.”
Now, with his first year as CEO complete, Mr. Wester sees tremendous opportunities ahead.
Moving from Healthcare to Health

Memorial Healthcare System was recognized by the Sheriff’s Foundation of Broward County for its sponsorship of the 6th annual Broward Mental Health Summit. Pictured here, from left: Broward Sheriff Gregory Tony; Tim Curtin, Memorial Executive Director of Community and Youth Services; and summit leader Beth Tache
While all healthcare providers serve patients and families when they are sick, Memorial is centered on moving to a higher level of care, Mr. Wester says.
“Because we are community-focused and community-connected, we seek our needs and gaps of care and fill them,” he says. “In addition to preventive care and acute care, this higher level promotes health and wellness throughout patients’ lives, with Memorial as their trusted base of knowledge.”
Memorial is reaching out beyond traditional care to improve social determinants of health — risk factors that can have an adverse impact on patients’ well-being, such as lack of access to healthy food, easy transportation, safe housing or even their own medical records.
Memorial Primary Care and Memorial’s Community Services are actively addressing these and other issues like mental health, substance abuse and domestic violence, to reduce the negative impact of non-medical causes of illness and chronic conditions.
“Of all the partnerships Memorial has, the most important one is the commitment we give to families for their long-term health and well-being,” Mr. Wester says.
Improving access to care
Memorial is expanding access to care by building healthcare “hubs” of various sizes in key areas of Broward, based on community needs.
“Navigating healthcare in a market like ours is a real challenge,” Mr. Wester says. “Because of that, people can delay the type of care they need and then ultimately end up in the Emergency Department. Healthcare hubs will help prevent that by improving access.”
The hubs — facilities with different combinations of healthcare services — will vary in size and scale, depending upon what providers are nearby. For example, a small health hub could offer primary, specialty and urgent care, all in one location. A medium hub could add outpatient services and a freestanding ED, while a large hub would also include an ambulatory surgical center.
“With hubs, we’ll be pushing clinical care out into the community,” Mr. Wester says. “It’s all about access, access, access.”

Children’s Mobile Health Center
Reaching vulnerable populations
After decades of providing care at its hospitals and facilities, Memorial is bringing care, services and resources via targeted population health initiatives. For example, the One City at a Time program will focus for the next two years on Hfour cities where some of Broward’s most vulnerable residents live. Memorial will send out mobile units once a week to provide vaccines, screenings, physicals, nutritional counseling and more.
With initiatives like One City at a Time, Memorial is bringing key community stakeholders together to identify areas of greatest need, Mr. Wester says. “The program is very metric-driven and will really help us move the needle on population health and well-being,” he says.

(Top left) Memorial Primary Care physicians and practitioners prepare and distribute food and toys for the community; (Bottom left) Joe DiMaggio Children’s Hospital staff providing supplies to Pine Crest School Community Service & Special Programs; (Right) Four new floors at Joe DiMaggio Children’s Hospital
Continuing to build Memorial’s pediatrics services
After a year that celebrated four new floors at Joe DiMaggio Children’s Hospital and the addition of six pediatric specialty services at Memorial Hospital Miramar, Memorial will continue to build its pediatric clinical programs and access locations, Mr. Wester says.
“I think it’s really the acknowledgement that Memorial is the largest provider of pediatric care in South Florida,” he says. “We’re building a depth of clinical care in this area that no one else can replicate.”
Celebrating community support
While Memorial has built several key strategic affiliations with other providers, one of the most critical partnerships is with its own community, which provides generous funding and outside support.
“We honor the contributions of our community leaders and donors who have clearly demonstrated their belief that Memorial is a great partner for their needs and interests,” Mr. Wester says. “We want and need their voices at the table. We’re not egotistical. We respect and value the input of our stakeholders from outside our organization.”

Leadership meeting with CEO K. Scott Wester (at head of table) at Memorial Regional Hospital South
Continuing to lead in a time of change
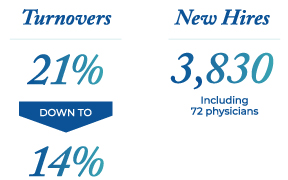
It’s been an extraordinarily transformational period for both healthcare and Memorial. In recent years, Memorial faced a once-in-a-century pandemic, saw 70 percent of its executive team take new assignments or retire, and lost frontline employees to retirement, burnout or traveling work.
Yet Memorial has stayed at the top of its game — recognized both statewide and nationally not just for its ability to weather COVID-19, but for taking the lead on what healthcare will look like over the system’s next 70 years.
Chairman of the Board of Commissioners Brad Friedman sees Memorial’s people as the ultimate key to that success.
“Memorial’s culture has always allowed us to attract great talent,” he says. “We’ve sustained ourselves through our recent changes and challenges because of the people at the core of the system who care about our mission. Memorial is moving confidently into the future because we’ve shown that we are all capable of accomplishing anything we have to.”
Mr. Wester agreed.
“Memorial’s strengths are due to our leaders and employees who are dedicated to supporting all health relationships, to having a lasting impact on people’s lives and to always leading through ideas and action,” he says.