Brett Rose and his family were returning from a well-earned vacation in the Florida Keys when he noticed strange blotches developing over his body. When he woke up at home the next day, he couldn’t walk. His husband, Jerry, had to carry him downstairs and take him to the ER at Memorial Regional Hospital South.
They knew Memorial well, thanks to Brett’s service on Memorial and Joe DiMaggio Children’s Hospital boards and his leadership on the Catch the Love campaign. But it was July 2020 — and like the rest of the world, Memorial was in the middle of the first wave of COVID-19. Jerry had to leave Brett at the ER, unable to follow him in.
It was just the beginning. Brett spent the next six months in the hospital, the victim of a mosquito bite that gave him West Nile, meningitis, encephalitis, Zika and dengue — “the ultimate concoction,” as he puts it.
“You’ve heard of the billion-dollar lottery?” Jerry says today. “That’s what this was — his one in a billion chance. He can’t win the lottery, but he gets this!”
The combination of infections and his immune system’s response had damaged the spinal cord and led to quadriparesis for Brett, meaning his arms and legs were weakened and his mobility impaired.
“Quite frankly, at the time, I was scared,” Brett recalls, “because that’s when the reality of what was my new life hit me: Hey, I can’t get out of bed. I can’t put my socks on.”
Journey to Recovery
When Brett was admitted, Joanne Delgado-Lebron, MD, felt a bit overwhelmed.
“He had one of the worst clinical presentations of West Nile you can have, plus encephalitis, meningitis and the neuromyelitis,” she says. “It was different from other types of spinal cord injury or neuro diagnoses we commonly see.”
While Brett doesn’t remember much about this time, Jerry vividly recalls the stress he and his family experienced, but Memorial’s caring and compassion made a true difference.
“Never once did I not have a brother or sister at Memorial,” he says. “Never once did I feel like I was in the dark. Every single doctor and nurse answered my questions — sometimes two, three, five times a day.”
After four weeks in the ICU, Brett was well enough to enter rehabilitation, where the hard work really began.
“Brett really wanted to get back to where he was. He had a very happy life, a very rich family life, great work life,” says James Salerno, MD, Chief, Physical Medicine and Rehabilitation.
"In spite of his situation, Brett refused to be pessimistic,"" Dr. Delgado-Lebron says.
“One of the main things that helped was Brett’s personality,” she says. “He was always very positive and compliant with the therapy, which was good because when you have West Nile and neuromyelitis, it can go either way.”
Brett is a symbol of what Memorial is able to do. To see patients on their first day, when they’re feeling hopeless, and then see those same patients walk into your office months after completing their therapy, living their usual lives — that warms my heart.”

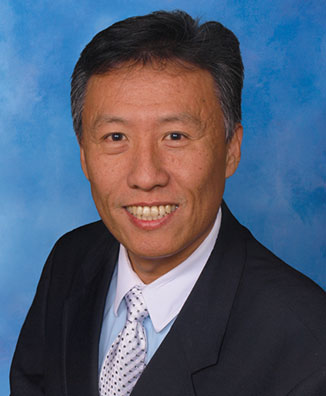
Joanne Delgado-Lebron, MD
Associate Program Director, Physical Medicine & Rehabilitation Residency Program
Memorial tailored Brett’s rehabilitation program specifically to his needs, to help him achieve each of the milestones he and the team set. With each goal he reached, the care team expanded the plan to help him achieve even more.
“He had a severe injury and required a lot of help, but he was very diligent and hardworking,” says Dr. Salerno. “And because of all the different aspects of care that Memorial Rehabilitation Institute puts on the table — like certified specialists in brain injury therapy that a lot of other centers don’t have to the degree we do — we were able to help Brett achieve the recovery he wanted.”
Brett underwent physical therapy for 20-plus hours a week as both an inpatient and outpatient. After his discharge, Rich Gach, PT, DPT, visited Brett’s home regularly to provide more therapy. “Seriously, it was the most wraparound healthcare imaginable,” Jerry says.
Drs. Salerno and Delgado-Lebron think of Brett as one of Memorial’s most remarkable success stories.
“Brett is a symbol of what Memorial is able to do,” Dr. Delgado-Lebron says. “To see patients on their first day, when they’re feeling hopeless, and then see those same patients walk into your office months after completing their therapy, living their usual lives — that warms my heart.”

Brett and physical therapist Kantica Arora, DPT
Members of the Family
The story of Brett’s rare illness and recovery is an example of the outstanding healthcare that patients receive at Memorial, from acute care to rehabilitation. It also sums up Memorial’s approach to transformational, 360-degree care — because while Brett is back to functioning at nearly 100 percent, Memorial remains a part of Brett and Jerry’s family and will continue to touch them throughout their lives.
“Memorial truly owns our experience,” Jerry says. “We can’t thank them enough for what they’ve given us. We’ve made friends for life there.”
I really got to experience almost every facet of the Memorial system,” Brett says. “I don’t think there was an MRI, CT scan or other test that I didn’t go through. I had an amazing team between cardiology, neurology, occupational therapy, general medicine and pulmonology. I got to experience the system at its finest.”
Brett Rose
Ft. Lauderdale

Brett with rehabilitation nurse Irma Valencia, RN; occupational therapist Carly Sheppard, OTR-L; and physical therapist Kantica Arora, DPT.